Let’s get the FREE stuff out of the way first.
These summaries are meant to be a gateway into the subject for people that don’t have time to read whole books. But they are NOT a substitute for the book as there is so much wonderful stuff left on the cutting floor. I encourage you to buy, share and gift Heather Fraser’s amazing book to anyone curious about why their child has an allergy (not just to peanuts).
The Peanut Allergy Epidemic: What's Causing It and How to Stop It-Fraser, Heather
You can now also listen to the article.
It’s good to see Dr. Kory in the masthead video, fighting the good fight. Both he and Kirsch have become incredibly valuable voices in the childhood vaccination battle.
I’ve been staring at this Allergy subject for so long, not quite sure what to write.
It is both so simple, and so complex.
Let’s stick with the really simple first.
Childhood vaccination causes allergy.
You can stop reading now and pack up, that’s it, mystery solved.
If you do not want a child with allergies, the first step is to not vaccinate them. If you need proof of this point, please watch the last 20 minutes of Vaxxed 2, here.
The Unvaccinated - Lies are Unbekoming (substack.com)
Now moving on from the really simple, to the simple:
Childhood vaccination causes allergy.
How it causes allergy has been known for over 100 years.
Injecting something into the blood stream is fundamentally different to ingesting it.
Allergy is not a disease but the body’s last-ditch attempt at a defensive response to expel a toxin.
I remember years ago, when our kids where in kindergarten and primary school, my wife and I would have conversations about all the kids (including our own) with all their allergies. I remember being convinced there must be a meta explanation, and I remember leaning towards a “processed food” explanation. But what I most remember is that it did not occur to me for one second that it might have anything to do with vaccination. That is how well my ignorance was constructed.
Now that I understand a thing or two about Empire and its Cartels, I can see what they have been up to in the allergy space. One of the aspects that I find most interesting when looking at cartels and their reality distorting “industrial marketing” or Propaganda, is just HOW they create that reality distortion.
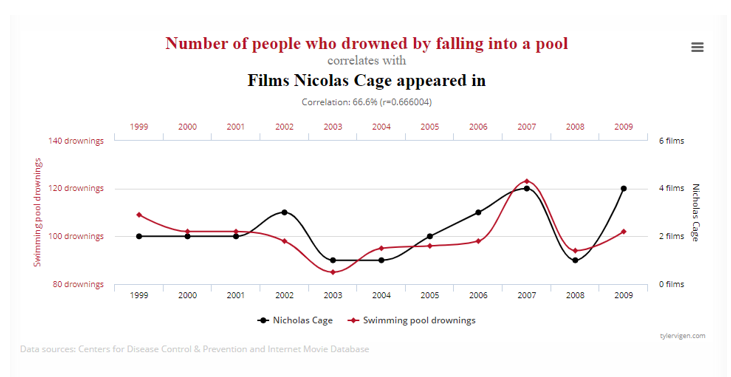
They use a multitude of strategies and often several at the same time. The main strategy they have used in the allergy space is “spurious correlation”, they look for any correlation that they can find and pump some money into studying it, and by “studying” so many different correlations they create so much doubt that it’s almost impossible to find your way through it.
One of my all-time favourite websites is:
Spurious Correlations (tylervigen.com)
This one for example shows the correlation between pool drownings and Nicolas Cage movies. Now it’s only a 66.6% correlation, but clearly something is going on.
Let’s have a look at some of what industry has been “studying” to try and solve the peanut allergy mystery.
Age of Onset
Birth Month
Gender
Race
Maternal Age at Delivery
Large Head Circumference
Heredity
Some of the usual suspects in the above list, such as “maternal age”, which is the allergist’s version of the ever reliable “blame the mother” strategy. And obviously genetics, that is always a safe one to “research”.
But my favourite, on par with the Nicolas Cage correlation is the “large head circumference” correlation. I am not making this up!
This section from Heather Fraser’s wonderful book:
LARGE HEAD CIRCUMFERENCE
Researchers in 1999 correlated the rise in allergy in children with the size of their heads. A study of newborn cord blood samples and measurements revealed an increase in IgE related to large head circumference. IgE is traditionally thought to be produced only by the mother and cannot pass to the child. While this idea is being reviewed in the literature the level of IgE in the mother is thought to be a means of predicting a risk of future allergic tendency in the child.
The explanation for the relationship between a large head at birth and future allergy was curious. In affluent societies where nutrition is generally good, researchers explained, the fetus will grow rapidly during the early stages of pregnancy and will remain programmed to grow at this rate. As the pregnancy progresses, the child will have a high nutrient demand, which is difficult to meet. In a poor community with poor nutrition, the fetus is programmed to grow slowly and have lower nutrient demand. The high-demand fetus is suddenly in a position where nutrient delivery is constant and therefore does not sustain growth. The brain and head continue to grow at the expense of the body that results in a big head and normal birth weight but poor nutrient delivery to other parts of the body. This, in turn, modifies the immune system. Apparently, the Th1 side is more susceptible to being switched off in adverse circumstances than Th2. Thus, it was suggested, the relationship of a large head and suppressed Th1 side explained the increase in allergy in affluent societies.
While having a large head at birth may point to future allergies, according to limited studies, it did not explain the sudden accelerated prevalence of peanut allergy starting around 1990.
So, there you have it. The explosion of peanut allergies “might” have something to do with large heads. We should definitely “research” this more. We should also research the correlation between peanut allergies and Nicolas Cage box office takes, I think there might be something there also.
Next, I want to share a section from Amelia’s as yet unpublished book on childhood vaccination, that she kindly shared with me some time ago.
Summary and Introduction
Did you know that to make bacteria and live virus vaccines, which doesn’t mean the virus is alive like us, it just means the vaccine contains the whole virus rather than fragments of the virus, they put the bacteria or whole virus in a soup containing a protein and the bacteria or virus is nourished by the protein and reproduces itself?
Did you know they sometimes nourish their bacteria and viruses with food that we eat?
They may put peanut oil in the soup and in some countries, children develop allergies to peanuts.
They may put sesame oil in the soup in Israel where some children develop allergies to sesame seeds.
I write “may” because they don't have to explain what they put into their soup, aka “culture medium”, because the soup ingredients aren’t supposed to be in the vaccine, they are supposed to be filtered out.
The reason for filtering out the soup ingredients is that the world has known since 1913 that if you inject a protein into the blood of a mammal (dogs were used) and later let that mammal eat that protein, the mammal can have a massive allergic reaction to that protein and die.
So how good is the filtering process?
Explanation
It is an important question because in many developed countries dramatic increases in the number of children with serious food allergies began in the 1990s and food allergies in children are now quite common.
For example:
an investigation of pre-schoolers showed a five-fold increase in serious food reactions in ten years. (R.J.Mullins ’Pediatric food allergy trends in a community-based specialist allergy practice 1995-2006’ Medical Journal of Australia 2007)
a study in the USA in 2011 involving 38,000 children found that 8% of children have a food allergy, 38% of whom have a history of severe reactions and 30% had multiple food allergies (Gupta et al, ‘The prevalence, severity and distribution of childhood food allergy in the US’ Journal: American Academy of Pediatrics, 2011).
it has been estimated that 220 – 520 million people may suffer from food allergies globally. (World Allergy Organisation: White Book on Allergy)
Charles Richet[i] got a Nobel prize in 1913 when he showed you can make a mammal allergic to a food protein by injecting that mammal with the protein. We are mammals, so this process is the same in us as it was in the dogs he experimented on. If a food protein gets into our blood without going through the normal digestion process our immune system recognises it as foreign and dangerous because food proteins don’t normally get into our blood in that form, undigested. Our immune system prepares itself so that the next time we have contact with that food protein, whether it is injected into us, or we eat it or touch it, our bodies try to defend themselves and this process can be harmful to us, in which case it is called an allergic reaction. The process by which our immune system discovers a food protein in our blood stream and labels it dangerous is called sensitisation.
No one disputes that over the last 30 years the number of cases of food allergy in children has risen dramatically in many developed countries. Many scientists have spent years researching the causes of food allergies and have wondered about what is causing this sensitisation to what are, normally, harmless food proteins. Here are some of the possible causes that have been investigated:
that life in developed countries has become more hygienic
that people are getting less sunshine and less vitamin D
that diets have changed
that stress has increased
that the number of caesarean births has increased
None of these changes have provided a satisfactory explanation for the food allergy epidemic given its geography and timing.
Food proteins can be introduced into a baby’s blood by vaccines because often proteins we eat, instead of proteins we never eat, are used in the manufacture of vaccines. To make a large batch of bacteria, or “live” viruses, for vaccines they start with a small quantity and feed it something it likes so it will reproduce. This is no secret; the bacteria and viruses won’t reproduce without food.
When they have produced enough bacteria or virus to make a batch of vaccines, they filter out the food protein, so it is not included in the vaccine. But their methods aren’t 100% perfect, a tiny quantity of food protein is sometimes included in the vaccines.
Is the quantity sufficient to sensitise some of the people who receive the vaccine, leading them to develop an allergic reaction to that food?
In Japan in the 1980s they did some things that proved Richet was right and the science hasn’t changed. In 1988 a Diphtheria – Tetanus – Acellular Pertussis vaccine was introduced for babies which contained a food protein, refined gelatine. It was given to babies when they were three months old. The number of cases of gelatine allergy in children started to rise, some babies had serious allergic reactions, ‘anaphylaxis’, to the Measles – Mumps - Rubella vaccine, which also contained refined gelatine and was given to them when they were eighteen months old. Other babies had serious allergic reactions to foods which contained gelatine. The Japanese government concluded that the tiny amounts of gelatine protein deliberately injected into the babies in the DTAP vaccine was causing the subsequent allergic reactions to the MMR vaccine and to gelatine in food. The gelatine was then removed from the DTAP vaccine. The number of cases of allergies towards gelatine dropped again.
An Australian paediatric allergy expert, Doctor Susan Prescott, wrote a book ‘The Allergy Epidemic: A Mystery of Modern Life’ in 2011:
‘Some vaccines are cultured in chicken embryos (such as the Measles, Mumps and Rubella ‘MMR’ vaccine), and may contain minuscule amounts of egg protein.... (Influenza vaccines) are also derived from chicken embryos, but egg protein content can vary with different influenza vaccines.’
So she knows the filtering system isn’t perfect. Dr Prescott wrote that a child with an egg allergy can be given the MMR vaccine because the amount of egg protein in MMR vaccines is so small it would not provoke an allergic reaction. She does not give that advice for flu vaccines. Instead she wrote: ‘it is best that the parents of egg allergic children discuss this with their specialist.’
Nowhere in her book does Dr Prescott ask what to me is an obvious question: is it possible that the food proteins in vaccines is causing the food allergies in children in the first place? She wrote the amount of egg protein in flu vaccines “can vary”. I infer she means a child with an allergy to egg protein could have an allergic reaction if the brand of flu vaccine that child is given contains a large amount of egg protein. Flu vaccines are recommended for children as young as six months old.
If there is enough egg protein in some flu vaccines to cause an allergic reaction, is there enough egg protein in some flu vaccine to cause the allergy?
Heather Fraser, a mother of a child with a peanut allergy, also wrote a book in 2011: ‘The peanut allergy epidemic: what’s causing it and how to stop it’. She asked the question: is the dramatic rise in peanut allergies in children due to the use of peanut oil in the manufacture of vaccines leading to tiny quantities of peanut protein being present in the vaccines? As she explains, a lot of research has been done to see if the way people cook and eat peanuts or use peanut oil in moisturisers and other products can explain the huge rise in the number of children who are allergic to peanuts. No simple explanation has emerged. The one possible cause that has not been subjected to extensive research is the presence of peanut proteins in vaccines.
Do vaccines cause food allergies? It is another elephant in the room that GPs haven’t noticed.
This is a passage from Chapter 2 of Handley’s How to end the autism epidemic:
Vaccines Are Linked to Autoimmune Disease
While this book is specifically about autism, it’s important to point out that autism may just be the tip of the iceberg for a host of neurological and physical disorders impacting our children at epidemic levels. Conditions of autoimmunity —asthma, diabetes, food allergies, eczema, and so on—are growing at rates similar to autism. Could vaccines also be behind their explosion? According to many scientists, absolutely.
As one example, scientists at the University of Virginia have drawn a direct line between the aluminum (referred to as “alum”) used in vaccines to stimulate the immune system and the explosion in food allergies, stating “the era of food allergy began with the post-millennial generation, the same faction who received new immunizations during early childhood. Many of these vaccines contain alum, an adjuvant known to induce allergic phenotypes.”61 (As you will soon learn, aluminum adjuvant may explain much, much more.)
Allergy scientists know that if they want to create a food allergy in rats, the quickest way to do it is by injecting them with vaccine ingredients. In a study from Norway—“Development and Characterization of an Effective Food Allergy Model in Brown Norway Rats”—scientists wanted to figure out the quickest way to give lab rats a food allergy so they could study various food allergy suppression drugs on them.62 Since rats aren’t born with food allergies, the most effective method was clear: inject the rats with egg protein and aluminum adjuvant, and they will soon be allergic to eggs.
There’s even a textbook from one of the largest textbook companies in the world (Wiley & Sons) titled Vaccines and Autoimmunity, a book that “explores the role of adjuvants—specifically aluminum in different vaccines—and how they can induce diverse autoimmune clinical manifestations in genetically prone individuals.”63 The book’s coauthor, Dr. Yehuda Shoenfeld, is viewed as the world’s foremost authority on autoimmunity, and he is very direct in raising the alarm bell about vaccine side effects: “Due to the adverse effects exerted by adjuvants, there is no controversy over the need for safer adjuvants for incorporation into future vaccines.”
Here is the book that Handley is referring to: Vaccines and Autoimmunity.
A wonderful part of Heather Fraser’s book is her explanation of the history of the syringe.
Injection bypasses the digestive tract that breaks down proteins, so they don’t elicit an immune response. The needle bypasses our natural defensives and delivers unprocessed proteins into the bloodstream.
This elicits an immune, sensitizing, response, which “loads the gun” so that when you then eat that protein, your immune system/body tries to expel it…an allergic reaction is a defense mechanism…not a “condition” or a disease.
As an Australian I’m always interested in Australian connection. This from Fraser’s book.
THE AUSTRALIAN EXAMPLE
The history of changes to the pediatric schedules in Tasmania and the Australian Capital Territory provided yet another provocative illustration of how and when peanut allergy emerged.
In a 2001 study, none of the 456 Tasmanian children aged seven to eight years reacted to a peanut skin prick test. By 2009, one in ninety children or 1.11% was allergic to peanuts. Changes in the vaccination schedule and the increased rate of children vaccinated in Tasmania correlated to this development.
In 1997, Tasmanian children were the least likely to be vaccinated at 27% of children according to the Australian Bureau of Statistics. Vaccination rates were dramatically low and declining on this island of about five hundred thousand people. In 1998, only 21% of children were vaccinated by their first year.
In 1998, the Australian government established a General Practice Immunization Initiative that intensified the pediatric schedule and national coverage for preschool children, including those in Tasmania. The goal was to have over 90% of the children vaccinated. In 2001, the Australian government implemented their strategy and surpassed their goal by vaccinating 94% of Tasmanian children by age one. Tasmania became the highest vaccinated population in the country. By 2009, 1.11% of Tasmanian children were allergic to peanuts.
In contrast to the sudden growth of the allergy in Tasmanian, peanut allergy in children living in the Australian Capital Territory (ACT) grew steadily. By 1995, 0.5% of ACT children were peanut allergic. By 2001, 0.71% of ACT children were allergic, and by 2009 2% of “school entrant” ACT children were confirmed as peanut allergic. Children living in this national political center were the most likely to be fully immunized at 48% in 1995 according to the Australian Bureau of Statistics. Changes to the pediatric schedule of ACT were similar to but made less rapidly than those in the United States and the United Kingdom. The changes to the schedules for ACT and Tasmania were, of course, the same. But again, the primary difference between Tasmanian children and those living in ACT was vast differences in rate of vaccination. Government programs attempted to harmonize this rate in 2001.
Here is a summary of the abstract from the Vinu Arumugham paper:
Abstract Summary:
Nobel Laureate Charles Richet established over a century ago that injecting proteins into organisms can cause sensitization, leading to allergic reactions or anaphylaxis. This has been repeatedly confirmed, most authoritatively by the Institute of Medicine (IOM) in 2011. Many vaccines contain food proteins, which have been shown to cause sensitization since 1940. However, allergens in vaccines are not fully disclosed, and there is no regulation for safe dosage levels or allergen quantities in vaccines and excipients.
A smaller amount of allergen is needed for sensitization than elicitation, and many approved vaccines contain enough allergens to cause anaphylaxis. Factors such as fewer childhood infections, less exposure to helminths, a 50% increase in C-section births (leading to sub-optimal gut microbiome), and the use of adjuvants in vaccines contribute to an immune imbalance towards atopy[ii].
Today's vaccine schedules include 30-40 shots, with up to five shots administered simultaneously, containing adjuvants like pertussis toxins and aluminum compounds that bias towards allergy. This combination, along with the injection of food proteins, contributes to millions developing life-threatening food allergies.
What I find interesting is just what you need to do nowadays to get published. If you are going to get something published, that hovers over truth (that is not in line with the Official Story) then you absolutely need to take the knee and bow to The Church with nods to “approved” Secondary Official Stories.
In the above Vinu gives a nod to:
The Hygiene Hypothesis[iii] - “Factors such as fewer childhood infections”
The Helminth Hypothesis[iv] (a derivative of The Hygiene Hypothesis)- “less exposure to helminths”
Mother blaming – “a 50% increase in C-section births (leading to sub-optimal gut microbiome)”
Genetics – “to an immune imbalance towards atopy”
There is enough confusion here to allow Vinu to mention adjuvants and proteins.
Here are some excerpts from Fraser’s book and Summary with some commentary from me:
Most scientists understand the radioactive peril of raising questions that implicate vaccine safety. Scientists, like doctors and journalists, know that vaccine debate can be a career-ending minefield. For that reason, scientists interested in allergies tend to cluster around safe harbors like genetic studies or behavioral research.
We know that genetics is a go-to cover story, but “behavioral research” is another effective tool that is used to protect Official Stories.
A great example in the allergy space is the study of the Nocebo Effect[v] (this is high quality victim blaming) as the suggestion is that a patient’s “concerns” might be the cause of their problems.
Adjuvants promote allergic sensitization not just to vaccine antigens, but also to other “bystander” proteins and allergens in the ambient environment at the time that the adjuvanted vaccines were administered.
-
An important and clear distinction must be made between sensitizing someone to peanut and launching the allergic reaction. Sensitization is believed to occur when a protein bypasses the detoxifying process of the digestive system and becomes bonded with blood serum. A healthy digestive system will neutralize any potentially sensitizing protein.
The reason why it’s been so easy to create confusion in the allergy discussion, is because there is a one-two process that begins with Sensitization[vi], that happens on the quite. It’s a multi-step process[vii], that is complex, and within that complexity, and delayed reaction, they have been able to create plenty of confusion with spurious correlation.
The homology[viii] between proteins in the Hib vaccine and peanuts raised concerns about cross-reactivity and sensitization to allergens.
Besides the use of actual peanut oil in vaccines, they use proteins that are “homologous” to peanuts. Or in English, very similar, or so similar that it sensitizes the system to a broad range of proteins that have a similar structure.
In fact, a 2006–2007 study stated that it did not matter whether mothers ate peanuts or not—the same percentage of children developed the allergy.
Said another way: Injection vs Ingestion.
Sweden, which has a low level of peanut consumption, has a higher prevalence of the allergy than the United States. Israel, which has a high level of peanut consumption, has a low prevalence of peanut allergy in Jewish children at 0.6% in 2012 (but a high prevalence of sesame allergy) and a high prevalence of peanut allergy in Arab children (2.6%) living in the same country.
-
From this mound of information, doctors have developed and tend to favor two explanations for the current epidemic of peanut-sensitized children. They are the helminth hypothesis and the hygiene hypothesis.
-
From this observation, researchers developed an explanation for all allergies: because parasites and humans have coevolved, they have an apparent symbiotic relationship in which parasites suppress allergic reactions while enjoying their human host. Without worms, the theory states, humans are unable to achieve homeostasis. In other words, immune dysfunction occurs due to lack of worms.
Said another way; hygiene, which is the very reason why childhood diseases have virtually evaporated (read Dissolving Illusions) has been blamed for the emergence of allergy. It’s such wonderful, twisted logic.
So, you are either living a life that is too clean, or you don’t have enough worms in you (helminth hypothesis). Those are the two most likely Official Stories according to The Science.
Another popular explanation for the rise in childhood allergies grew from an apparent correlation between this rise and the general decline in family size. It was proposed that unhygienic contact in large families—lots of siblings bringing illness home from school—was important for the development of a healthy immune system. The greatly expanded and much-touted hygiene hypothesis suggests that overzealous cleaning, germ-killing products, chlorinated water, antibiotics, (vaccination is specifically avoided by researchers) have “protected” Western children unnaturally. And as a result, the immune systems of First World children, in particular, are sheltered from a natural microbial burden. Their immature immune systems are understimulated, dysregulated, and therefore prone to random allergic sensitization. This malfunction is a product of an unburdened lifestyle.
Here, you are not having enough children. If only you had a larger family, you wouldn’t have all these children with allergies.
In addition, these two favored explanations for the epidemic assume that allergy is a dysfunction, that the body has made a mistake in attacking a benign substance. And yet, the opposite may be true. Some suggest that allergy has an evolved purpose seen before the twentieth century but provoked increasingly today by drugs and noxious pollutants in our air, water, and food.
-
The scratching, vomiting, diarrhea, and sneezing are desperate attempts to eject a toxin as fast as possible. It is a risky reaction but one the body is programmed to unleash as a last-ditch effort to protect itself. This event occurs when the general defenses have been insufficient in preventing a specific toxin from accessing the bloodstream for a second time.
-
Conspicuous by its absence from current theories is the one mechanism that has an actual history of creating mass allergy—injection. Injection is examined in this book in some detail since it was the means by which the founder of anaphylaxis, Dr. Charles Richet, stumbled on alimentary (food) anaphylaxis in humans and animals over one hundred years ago. Richet concluded in 1913 that food anaphylaxis was a response to proteins that had evaded modification by the digestive system. Using a hypodermic needle, he was able to create the condition in a variety of animals—mammals and amphibians—proving that the reaction was not only universal but also predictable using the method of injection followed by consumption or another injection.
-
These cross-reactive proteins may include those in the Hib cellular membrane or legume oil in a popular brand of the vitamin K1 prophylaxis. Cross-reactivity explains why a person who is allergic to peanuts, legumes like soy and castor beans, may also react to nuts or citrus seeds, which belong to different plant families—their proteins have similar molecular weights and structures.
-
The chapter also mentions the introduction of a vitamin K1 prophylactic injection for newborns, which contained potentially allergenic ingredients. During this same period, there was an increase in peanut and food allergies among children, leading to a concerning rise in severe food allergies.
-
To overcome these obstacles to compliance with the new schedule, the vaccines for diphtheria, pertussis, and tetanus (DPT); polio (OPV); and H. influenzae b (Hib) were administered to children in a single visit with two injections and an oral polio dose starting around 1988. By 1994 starting in Canada, these five were rolled into a single needle. Few parents realize that by design, immunization provokes both the desired immune response and allergy at the same time. These natural defenses are inseparable and the more potent the vaccine, the more powerful the two responses. This is an outcome of vaccination the medical community has understood at least since Charles Richet won the Nobel Prize (1913) for his research on anaphylaxis. Anaphylaxis, Richet observed, is one of three outcomes of vaccination.
What has emerged, instead, is a robust economy of doctor fees, nut-free foods, ongoing medical research, and pharmaceutical sales. Peanut and other food allergies have become enormously profitable. It is so much so that one market analyst has suggested that an “autoimmune index” would be a great tool for investors. This index, tagged as “save the children and make money,” would monitor the profitability of pharmaceutical stocks relative to the continued rise in peanut allergy and other childhood epidemics.
-
Anaphylaxis, allergies, and serum sickness became prevalent with the mass application of vaccinations using hypodermic syringes in the late 19th century.
-
Mass administration of injected sera caused serum sickness, leading to the study of altered reactivity, later termed "allergy."
-
The hypodermic syringe and mass injections contributed to the first man-made allergic phenomenon in children, known as serum sickness.
-
Dr. Monroe J. Romansky innovatively used peanut oil in the penicillin formula, extending its duration and allowing for single daily injections.
-
The chapter (5) also discusses the use of vaccine adjuvants, specifically Adjuvant 65-4, which contained peanut oil and was used in flu vaccines in the late 1960s.
Allergy is the new name they have given the phenomenon.
They used to have an older name for it, “serum sickness”, which has today been rebranded.
What you will learn in Fraser’s book is that peanut allergy (serum sickness) is an old story that goes back to the use of peanut oil in penicillin, which created plenty of problems.
The motivation to use peanut oil in penicillin allowed them to use less penicillin per patient as it wouldn’t be flushed out of the system as quickly. Penicillin was expensive, so peanut oil use had significant economic advantages.
It’s the same story now with vaccines.
The addition of peanut oil allows them to use less antigen (biological matter) per dose. Antigen is expensive. So, it’s economics again.
Thanks for being here.
Please consider a small paid subscription (donation). The money goes to help covid vaccine injured Australians.
I am always looking for good, personal GMC, covid and childhood vaccination stories. You can write to me privately: unbekoming@outlook.com
If you are Covid vaccine injured, consider the FLCCC Post-Vaccine Treatment
If you want to understand and “see” what baseline human health looks like, watch (and share) this 21 minutes
If you want to help someone, give them a book. Official Stories by Liam Scheff. Point them to a safe chapter (here and here), and they will find their way to vaccination.
Here are three eBooks I have produced so far:
FREE eBook: A letter to my two adult kids - Vaccines and the free spike protein
[i] Charles Richet was awarded the Nobel Prize in Physiology or Medicine in 1913 for his work on anaphylaxis. He discovered the phenomenon of anaphylaxis, which is a severe, potentially life-threatening allergic reaction that can occur rapidly after exposure to an allergen. Richet's discovery has been crucial for understanding the immune system and its response to allergens, and it has contributed significantly to the development of allergy treatments and prevention strategies.
Here are some key points that we have learned from his work:
Anaphylaxis: Richet discovered the phenomenon of anaphylaxis, which is a severe, rapid, and potentially life-threatening allergic reaction.
Hypersensitivity: His work helped establish the concept of hypersensitivity, in which the immune system overreacts to harmless substances, leading to various allergic reactions.
Type I Hypersensitivity: Anaphylaxis is classified as a Type I hypersensitivity reaction, which involves the release of histamine and other inflammatory mediators from mast cells and basophils.
Role of antibodies: Richet's work contributed to the understanding of the role of antibodies (IgE) in mediating allergic reactions. This knowledge has been crucial in the development of allergy treatments.
Desensitization: His research led to the development of desensitization or allergen immunotherapy, a treatment that helps increase the body's tolerance to specific allergens.
Preventive measures: Richet's discovery of anaphylaxis has also helped devise preventive measures, such as the use of epinephrine auto-injectors (EpiPen) to counter severe allergic reactions.
[ii] Atopy is a genetic predisposition to develop allergic diseases. People with atopy are more likely to have one or more allergic disorders, such as eczema (atopic dermatitis), allergic rhinitis (hay fever), allergic asthma, or food allergies.
The term "atopy" comes from the Greek word "atopos," meaning out of place or unusual. It refers to the tendency to produce an exaggerated immunoglobulin E (IgE) response to otherwise harmless substances in the environment, such as pollen, dust mites, or certain foods.
In individuals with atopy, the immune system mistakenly identifies these substances as threats and triggers an allergic response. This can lead to various symptoms, ranging from mild, such as sneezing and itching, to more severe reactions like anaphylaxis.
Atopy often runs in families, and a person with a family history of allergic diseases is more likely to develop atopic conditions themselves. The interplay between genetic factors, environmental exposures, and the immune system's response contributes to the development and expression of atopic diseases.
[iii] The Hygiene Hypothesis is a theory that suggests a link between overly clean environments and the increase in certain immune-related disorders, such as allergies and autoimmune diseases. According to this hypothesis, exposure to various microorganisms, especially during early childhood, is essential for the proper development of the immune system.
The idea is that in modern, Westernized societies, where cleanliness and hygiene are highly emphasized, children are not exposed to as many bacteria, viruses, and other microbes as they were in the past. This lack of exposure might prevent the immune system from developing a proper balance between different types of immune cells, particularly the Th1 and Th2 cells.
Th1 cells are associated with fighting infections, while Th2 cells are linked to allergic responses. In the absence of sufficient microbial exposure, the immune system may become skewed towards a Th2 response, making individuals more prone to allergies and other immune-related disorders.
The hygiene hypothesis is often cited to explain the rise in allergies and autoimmune diseases in industrialized countries and has led to ongoing research and debate. Some evidence supports the idea, while other research points to more complex interactions between genetics, environment, and immune system development. It's also worth noting that the hypothesis has evolved and become more nuanced over time, recognizing the role of specific types of microbial exposures and the timing of these exposures in immune system development.
[iv] The Helminth Hypothesis is a theory that suggests a link between the decrease in parasitic worm (helminth) infections and the increase in immune-related disorders like allergies and autoimmune diseases in developed countries.
According to this hypothesis, parasitic worms have coexisted with humans for thousands of years, and our immune systems have evolved to accommodate these parasites. Helminths can modulate the host's immune response to prolong their survival within the host. This modulation may lead to a suppression or regulation of unnecessary immune responses, such as those found in allergies and autoimmune diseases.
In developed countries, improved sanitation, medical interventions, and lifestyle changes have led to a reduction in helminth infections. This decrease might have unintended consequences on the immune system, leading to an imbalance that favors inflammatory responses.
The Helminth Hypothesis is somewhat related to the Hygiene Hypothesis but focuses specifically on the role of parasitic worms. While the Hygiene Hypothesis considers a broader range of microbial exposures, the Helminth Hypothesis focuses on how the eradication of these specific parasites might contribute to the increase of allergic and autoimmune disorders.
Research in this area has led to experimental treatments for some autoimmune diseases using controlled and deliberate infection with specific helminths. Some studies have shown promising results, but this is still an area of active research and debate.
[v] The Nocebo Effect is the opposite of the placebo effect. While the placebo effect refers to a positive response to a treatment that doesn't have therapeutic effects, the nocebo effect refers to negative symptoms that arise from a harmless treatment due to a patient's negative expectations or beliefs about the treatment.
Here's how the nocebo effect might work:
Expectation of Harm: A patient is told that a particular treatment might have certain side effects or hears negative information about the treatment elsewhere.
Belief and Anxiety: The patient begins to focus on or worry about these potential side effects, becoming anxious or fearful.
Physical Symptoms: Due to the expectation and anxiety, the patient starts to experience the anticipated side effects, even though the treatment itself isn't causing them.
Reinforcement: The appearance of these symptoms can reinforce the belief that the treatment is harmful, potentially leading to a cycle where the symptoms persist or even worsen.
The nocebo effect shows the power of the mind in health and well-being. It highlights how a patient's beliefs, perceptions, and psychological state can significantly influence their physical experience. This phenomenon poses challenges for medical practitioners in terms of informed consent, communication, and patient management, as the way information is presented to the patient can influence both placebo and nocebo responses. Understanding and managing these effects can be crucial for the success of medical treatments and patient satisfaction.
[vi] Sensitization is a process by which the immune system becomes hyperresponsive to a specific substance, often called an allergen. Upon initial exposure to the allergen, the immune system may recognize it as foreign and produce antibodies against it, even though the substance might be harmless. This initial phase doesn't usually produce noticeable symptoms but sets the stage for potential allergic reactions in the future.
Here's how the process typically works:
Initial Exposure: Upon first contact with an allergen, the immune system triggers specific immune cells called B-cells to produce IgE (Immunoglobulin E) antibodies that recognize that particular allergen.
Binding to Mast Cells: These IgE antibodies then attach themselves to immune cells called mast cells, found in connective tissues throughout the body, including the skin and the linings of the lungs, stomach, and heart.
Subsequent Exposure: If the individual is exposed to the allergen again, the allergen can bind to the IgE antibodies on the mast cells' surface. This binding triggers the mast cells to release inflammatory substances like histamine.
Allergic Reaction: The release of histamine and other chemicals causes various symptoms of an allergic reaction, such as swelling, redness, itching, and potentially more severe symptoms like anaphylaxis.
Sensitization is the reason why an individual might not experience an allergic reaction upon first exposure to an allergen but may have a reaction upon subsequent exposures. It's a fundamental concept in understanding allergies and plays a critical role in allergy testing, where small amounts of potential allergens are introduced to see if the body has produced specific IgE antibodies against them.
[vii] An allergic response is a complex process that involves several steps. Here's a breakdown of the typical sequence of events that can lead to an allergic reaction:
1. Sensitization:
Initial Exposure: The body is first exposed to an allergen, recognizing it as foreign.
IgE Production: B-cells produce Immunoglobulin E (IgE) antibodies specific to the allergen.
Mast Cell Binding: The IgE antibodies bind to mast cells and basophils, priming them to react to future exposures.
2. Subsequent Exposure:
Allergen Binding: Upon re-exposure, the allergen binds to the IgE antibodies on the surface of the mast cells and basophils.
Mast Cell Activation: The cross-linking of the IgE antibodies by the allergen triggers the mast cells and basophils to release their contents.
3. Immediate Response:
Release of Mediators: The mast cells and basophils release preformed mediators such as histamine, leading to immediate symptoms like redness, swelling, itching, and bronchoconstriction.
Synthesis of Other Mediators: They also synthesize new mediators like leukotrienes and prostaglandins that contribute to the allergic response.
4. Late Phase Reaction:
Recruitment of Other Immune Cells: Hours after the initial reaction, other immune cells like eosinophils, neutrophils, and lymphocytes are recruited to the site.
Chronic Inflammation: The ongoing activity of these cells may lead to chronic symptoms and tissue damage, often seen in conditions like asthma or chronic hives.
5. Resolution or Escalation:
Symptom Resolution: With mild allergies and appropriate treatment, symptoms may resolve on their own.
Escalation to Anaphylaxis: In severe cases, the reaction may progress to anaphylaxis, a life-threatening allergic reaction involving multiple organs.
[viii] In the context of allergies, Homology typically refers to the similarity in structure or sequence between different proteins or allergens. This similarity can cause cross-reactivity, where antibodies produced in response to one allergen also recognize and react with other allergens that have similar structures. This can explain why some individuals who are allergic to one substance may also experience allergic reactions to other seemingly unrelated substances.
Here's how it might work in the context of allergies:
Initial Sensitization: An individual becomes sensitized to a specific allergen, such as a protein found in a particular type of pollen.
Cross-Reactivity Due to Homology: Other proteins in different pollens, foods, or substances may have similar structural features (homology) to the original sensitizing allergen.
Allergic Reaction to Different Substances: Because of this homology, antibodies produced in response to the original allergen may also recognize and bind to these other proteins, leading to allergic reactions when exposed to different substances that contain these similar proteins.
For example, someone allergic to birch pollen might also experience allergic reactions to certain fruits, like apples or cherries, because the proteins in these fruits are structurally similar to those in birch pollen. This phenomenon is sometimes referred to as Oral Allergy Syndrome or Pollen-Food Allergy Syndrome.
Understanding homology between different allergens is essential in allergy diagnosis and management, as it can help predict potential cross-reactive allergies and guide appropriate avoidance strategies and treatments.