Migraines aren’t a subject I’ve written about before.
I reached out to Jeff, and I’m very happy he agreed to do this in-depth interview on the subject.
With thanks to Jeff Baker M.D.
Natural Migraine Relief | Jeff Baker M.D. | Substack
1. Dr. Baker, can you please tell us about your journey in medicine? How did you go from a traditional medical background to developing an interest in integrative medicine and migraine management?
Thanks for the opportunity to interview with Unbekoming. In doing so, it looks like I am joining a very interesting tribe. Glad to be aboard!
I entered medical practice with the typical naïve enthusiasm of a young doctor, fuelled by the belief that through my training I had mastered the tools needed to solve most medical problems. It wasn’t long before I realized that too many of the medical “solutions” that I or my colleagues devised in the office or ER were incomplete, or too often short-term band-aids for problems that were deeper and more multi-factorial than met the eye. At the time I was practicing in Southern California, where it was not uncommon to hear from patients that wearing crystals, sleeping under a pyramid, or using an herbal cleanse were reasonable and competing treatment options to prescription drug therapy. As I have a borderline dangerous amount of curiosity, I began to investigate some of these non-conventional approaches to therapy and in the process discovered an entire community of both practicing and academic based physicians who were looking at a wide range of science-based approaches to the biomolecular origins of human cellular dysfunction. These included concepts and therapy considerations that I had never encountered in traditional medical training.
I began to attend meetings like those of the American College for the Advancement of Medicine (ACAM) where I learned from the pioneers of what we now call Integrative Medicine: Dr’s. Jonathan Wright, Richard Casdorph, Ted Rozeman, Julian Whittaker, Robert Rowen, Alan Gaby, Andrew Weil, William Campbell Douglass, and many others who wrote and lectured on using both pharmaceutical and non-drug options to manage the root causes of disease expression. Over the last 30+ years I’ve used these principles and techniques, along with appropriate conventional care options to address a wide range of health care problems in a private practice setting.
One of these interests has been the use of bio-identical hormone support for women throughout the reproductive life cycle. In the process of gaining the experience and expertise required to individualize hormone therapy, it became ever more common for me to hear a “oh, by the way, my migraines are so much better since I started this therapy” on follow up visits. While early in my practice I vaguely understood that hormonal influence played a role in migraine expression, this clinical experience where “balancing hormones incidentally helped migraines” sharpened my interest in learning more about that relationship. Over the last 10-15 years I have been more specifically looking for and managing hormonal and other “root cause factors” for migraine, which is the basis for my writing on that topic, which includes my blog, naturalmigrainerelief.substack.com, and my online course Natural Migraine Relief, which is at the same site.
2. You mention that migraines affect 1 in 10 people, but women are three times more likely to suffer from them. Why do you think there is such a significant sex disparity?
You’re right, the ratio for adult migraine is about female/male dominant at nearly 3 to 1, and an overwhelming number of women with migraine, some 70%, report a link between headaches and their menstrual cycle. It’s interesting, in contrast, that in childhood migraine the incidence is much higher in males (7 or 8 to 1) until the pubertal transition. Then the incidence flips, which is almost entirely reproductive hormone related. There are several female distinct hormonal patterns that are specific to promoting migraines that can explain this ratio, and I’ll cover some details on that in your next question.
3. Can you tell us more about the connection between hormones and migraines? How do fluctuations in estrogen and progesterone impact migraine occurrence?
It’s not so much the difference in levels between men and women, it’s the cyclic fluctuation in their levels, and the potential for imbalance in their ratios, especially estrogen vs. progesterone. One expression of this influence is how many women with migraine experience some improvement after menopause.
Here are four major elements of hormone influence in migraine that I find it useful to recognize and treat:
1. estrogen dominance, especially in the late (luteal) phase of the cycle. This is most commonly when there is a relative undersupply of progesterone, and estrogenic influence on inflammation and blood viscosity may be a contributory factor.
Migraines starting at puberty often have this feature. Estradiol only therapy for menopausal symptoms is a common therapy that may inadvertently load up that dominance effect. To avoid this, I prefer a topically applied estriol/estradiol ratio of ~70/30 or 80/20, matched with progesterone, and monitored with blood, urine, or salivary testing to use “the least amount of estrogen that gets the job done” for peri-menopausal and beyond therapy.
Avoiding estrogen dominance is probably the #1 hormone related intervention for migraine prone women. Because of this, throughout the menstrual cycle, and one’s life cycle for that matter, progesterone support is the mainstay of my hormone therapy recommendations when migraine is part of the picture.
2. a side issue to the estrogen dominance is how this situation can promote an excess of uterine prostaglandin production before and during the onset of menses. Prostaglandins promote smooth muscle contraction, which is an important part of initiating uterine shedding, but when produced in excess this can have an effect beyond the pelvis, affecting blood vessels elsewhere. This may include vessels that may be involved in blood flow changes at the initiation of a migraine. Blocking excess prostaglandin production with NSAIDs, like ibuprofen or naproxen, in the 24-48 hours prior to onset of flow can be a helpful tool for late cycle migraines that occur in sync with the onset of menstrual flow.
3. estrogen detoxification. There are downstream estrogen metabolites that have a pro-proliferative and pro-inflammatory effect. While reducing these metabolites may reduce breast specific problems like fibrocystic changes and even breast cancer, there is evidence that these metabolites may add to other pro-inflammatory drivers of vascular headaches. These metabolites can be assessed with urine metabolite testing like the DUTCH test, and reduced in proportion with the use of cruciferous vegetable extracts like DIM or indole-3-carbinol.
4. the other side of estrogen dominance is that of late cycle estrogen deficit. Some women with migraine have a drop in mid to late cycle estrogen. Estrogen can help moderate pain perception, and when it drops lower than usual can make the initiation of the migraine pain cycle occur more readily. Using low dose, late cycle estrogen may help alleviate that promoting factor. I would advise that for these patients, adding estrogen at any part of the cycle should be matched with bio-identical progesterone to avoid an inadvertent estrogen dominant component.
Female hormone factors are such a key root cause component that I find it rare to see migraines resolve unless they are considered and addressed appropriately.
4. In your experience, what are the most common misconceptions about migraines that you encounter?
So many out there, but here are three worth addressing:
1) a migraine is just a “real bad headache.” A migraine is a complex neurological event, in some cases having cumulative neurological and cognitive damage and deficits. It needs to be accurately diagnosed and treated with the root cause directed drug and non-drug interventions that are most specific to that patient.
2) Why can’t doctors cure migraines? It’s my opinion that this falls in the same category of “curing” Alzheimer’s, ALS and Parkinson’s. All of these are complex neurological disorders, with multiple promoting root cause factors including genetic expression, lifestyle habits, nutritional deficits, neurotoxins, and typically multiple sources of inflammation. In each case we should aim at 1) early detection and management, and 2) understanding the root cause factors specific to the individual with the disorder, with the goal of 3) managing the day-to-day expression of the problem as well as reducing long term progression.
Most of my migraine patients get a significant reduction of both intensity and frequency of their headaches. I’m not sure that I have many who were “cured”, as in “never had a migraine again, ever,” especially since it is so humanly common to lapse on the self-care that minimized the root cause contributors for their headaches in the first case.
3) the concept that finding and eliminating your ‘trigger factors’ is the key to migraine management. We see this a lot in clickbait type articles on FB or in health advice columns or blogs. I like to emphasize that trigger factors are rarely, if ever the underlying cause of one’s migraine. They are better described as “the tip of iceberg” in this process. Let’s go on to your next question which allows me to explain that better.
5. You talk about the "full cup" theory of migraine expression. Can you explain this concept and how it relates to trigger factors?
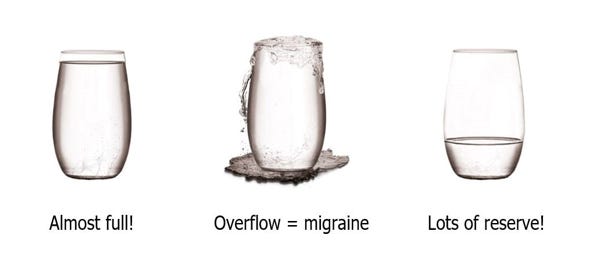
I find it useful to think of the clinical expression of a problem, such as the pain and disability of a migraine, as the overflow of an 8 oz cup.
Think of this filled cup and its overflow as being the direct manifestation of a migraine headache and its associated symptoms. One might ask, which of the eight ounces in the middle cup caused it to overflow? The right answer is: all of them.
Many people consider that last half ounce to be the ‘trigger’ that we think caused the migraine. The other underlying ounces are the root causes that fill the cup to where a seemingly casual trigger event is the last straw. That trigger could be a weather front, a certain food, glare from headlights, ‘that time of the month,’ seasonal pollens, an adverse smell or scent, or a dozen others.
But, if the cup is almost full most of the time, it doesn’t take much more to overflow. Anything could push it over the edge, multiple times a month and for multiple different “reasons.”
But, if we could identify your specific root factors and reduce the volume in the cup to only one, two or three ounces, we now have built in a reserve where it would then take a much larger volume of triggers, say five, six, or seven ounces in this example, to hit your headache threshold, if at all. That’s my approach to migraine: find and minimize the treatable root cause factors, build in reserve, and avoid overflowing the cup! See my FAQ Episode # 16: What is the cause of your migraines? Trigger factors vs. Root Cause factors for more details.
6. Your approach focuses on non-drug therapies. Why do you believe it's important to look beyond pharmaceutical solutions for migraine relief?
Apart from the CGRP inhibitor group, pharmaceuticals don’t typically treat or clear the specific root causes of migraine. They can modify the response or progression of a headache (like the triptan meds), or help to manage the symptoms of migraine, like pain and nausea. Complex problems like migraines rarely if ever have a “one silver bullet drug hits the cause-and-effect bullseye” solution. And as my colleague Robert Rowen puts it: “There is not a single chronic degenerative disease which arises from a deficiency of a synthetic petrochemical pharmaceutical.” (see his Unbekoming interview at Interview with Dr Robert Rowen.)
The root causes of migraine are the insufficiencies or interruptions of biochemical pathways that enable healthy function or the ability to repair readily when damage occurs. While drugs may at times fill a gap when this process is dysfunctional, many of the repair mechanisms respond to, and even require the restoration of native function. This is why therapeutic amounts of non-drug entities like CoQ10, riboflavin, Vitamin D, magnesium, progesterone, thyroid, methylated B vitamins, omega-3 fatty acids, thiamine, melatonin, pregnenolone, niacin or iodine can assist in clearing migraine headaches. At times we are making up for or working around genetic shortfalls that need a greater than average nutrient support.
My goal in is to be as comprehensive as possible in reviewing the indications and uses of these and many other agents of repair, both in my free Substack blog and my self-directed online course: Natural Migraine Relief (see Question 15 of this interview for details.) In this course covering 25 lessons we discuss ten major categories of root causes factors for migraine, along with 60+ associated co-morbid disorders and over 90 different interventions that help to minimize provocative factors that “fill the migraine cup” to overflowing.
7. You discuss the importance of vitamin D3 levels for migraine sufferers. What's the link between vitamin D deficiency and migraine frequency?
Vitamin D3 can play a neuroprotective role in several disorders including migraine, Alzheimer’s, and Parkinson’s. Several studies strongly suggest a direct link between Vitamin D deficiency and migraine expression.
One that illustrates this was done at the Migraine Center @ Cincinnati Children’s Hospital Medical Center, where they reviewed medical histories for 7,691 young migraine sufferers. They found that 70% of them had significantly lower vitamin D levels than the standard reference range. Another study comes from Denmark, where their latitude predisposes residents to Vitamin D deficits. It showed that when migraineurs with low Vitamin D were brought up to optimal levels, over half saw their headache attack frequency reduced by 50% or more.
I’ve found over the years that a very simple and effective adjunct for migraine therapy is to first check a Vitamin D level. And yes, like the Cincinnati study, I also find in my patients that around two-thirds of those with migraine have low (<30 ng/dl) levels. Our response to that is to load and adjust the daily Vitamin D dose to optimize the level. Just as in the Denmark study, I’ve also found that that augmenting levels to the 60-70+ ng/ml level correlates with clinical migraine improvement.
There are multiple algorithms for Vitamin D supplementation. I like the Grassroots Health Nutrient Research Center’s free and easy-to-use calculator for using your serum Vitamin D level to determine loading and maintenance doses.
Also see my blog post FAQ Episode 11: Migraine prevention: Make sure you don’t ‘fall back’ on your Vitamin D3 level for more information on this topic and references to the studies mentioned above.
8. Can you explain the role of homocysteine in migraines and why it's important for patients to have this level checked?
Homocysteine is a breakdown product of protein metabolism. Because it promotes inflammation, elevated levels of homocysteine have been associated with arterial plaques, brain aging, blood thickening or clotting and migraines, especially when there is an associated aura. If your family history is positive for migraine, heart disease, stroke at age <60 or dementia you should definitely check your homocysteine level.
A key factor in elevated homocysteine is the inability to activate three B vitamins that help to clear homocysteine. B6, B12 and folate (B9) must be chemically methylated to be activated to optimize this clean up function. You may have heard of the MTHFR gene group, which regulates methylation of B vitamins. More than 30% of Americans or Australians have a single gene defect here, and up to 10% have a more significant deficit. Since there are two gene sets involved and at least 40 related mutations that can affect them, it is useful to look past the genotypic coding to the phenotypic expression (what happens with the gene expression in “real life”) by looking at the homocysteine level as a clinical marker. A level of 6-10 mcmol/L would be optimal, 11-15 is possibly suspect and >15 is a level deserving attention.
Fortunately, nutritional therapy is inexpensive and works well to manage this gene deficit. You can readily the find methylated B combinations needed to cover this gap. Some people may also need extra methyl groups to get the job done. They can take the nutrient TMG (trimethylglycine) to achieve this. And, as red meat is rich in methionine, an amino acid that cycles in tandem with homocysteine, reducing red meat in the diet can help to reduce excess homocysteine levels.
If you would like to take a deeper dive on understanding methylation and homocysteine, take a look at the Substack article “It's all about methylation: everything you didn't know, you need to know, about methylation.”
9. You've written about the connection between thyroid function and migraines. How can addressing thyroid issues potentially help with migraine relief?
As a woman ages toward 50, studies estimate that she has somewhere between a 35-65% chance of having suboptimal thyroid function. They have shown that those with migraines are anywhere from 40-70% more likely to have low thyroid as a promoting factor than those without headaches. If you are in this group, especially with those with a gradually progressive autoimmune component, like Hashimoto’s thyroiditis, this trend may have started even earlier for you, perhaps even in your teens and 20s.
Let’s keep in mind that the “normal range” for any lab test is a Bell curve of functional expression. If you are “mid-range,” half of the population runs higher levels, half are lower. And at which part of this broad range are you “wired to run the best?” The answer is…nobody knows. Wouldn’t it be handy if we all came with a manual listing our “optimal settings” for any mode of function: thyroid output, testosterone level, blood pressure, % lean body mass for our build, ability to learn algebra, etc. But no dice. Never seen one.
So, when someone says they know what’s normal for you, they…are…guessing. OK, maybe an educated guess. If your 10th % tile level thyroid tests are “normal” for 10% of people, what if you are in the other 90%, or maybe even the top one-third? Aside from psychic intuition, how would you or your doctor know that?
Having a fix on “your normal level” could be immensely helpful, because thyroid is the metabolic sparkplug for every cell in the body and when thyroid support is lower than optimal, cellular energy deficits can be a key root cause for migraine headaches. If thyroid levels are augmented, along with key energy producing nutrients like magnesium, CoQ10, and riboflavin, the low energy state provocation of some migraines may be mitigated.
This is why I advise a trial of: 1) including the above noted nutrients in my “Basic Four*” to be taken initially by all my migraine patients, and 2) some version of iodine or low dose prescription thyroid support for those with either hypothyroid symptoms, low normal thyroid results and even low basal body temperatures (see blog post FAQ Episode 30b: Checking Basal Body Temperatures to assess the Thyroid/Migraine connection.)
The downside of a 60-90 day individualized and monitored trial as a “test drive” is minimal, and when these measures are key root cause factors, the resulting relief of migraine pain can be priceless.
* I’ve posted part of my paid subscriber course: Lesson 6: Integrative Therapy for Migraines for you to give some background and details on “The Basic Four.” Click the Lesson 6 link just above and after reading the first ~10 paragraphs you will see the dosing details for those four key nutrients.
10. You mention a potential link between migraines and Alzheimer's type dementia. Could you elaborate on this connection?
While we know that migraines share risk factors and brain changes with the four major types of dementia in general, prior studies hadn’t definitively proven that migraines cause dementia. A recent study from the Journal of Headache Pain study uncovered some interesting threads in this relationship. It reviewed seven longitudinal studies about migraine and brain aging, drawing from data gleaned from following over 200,000 individuals. The investigators looked at both the development of dementia over time and the changes found in MRI studies of the brain in those individuals.
The key conclusions were that:
a history of migraines may accelerate brain atrophy and the risk of dementia in the future.
a history of migraine with aura significantly increased the risk of Alzheimer’s type dementia and accelerated the annual atrophy of the total cortical surface area and thalamic volume.
If you have migraines with an aura and/or a family history of migraines, as well as dementia this is concerning news. If this is true for you, one of the most important things to do is to address the topic of the previous question, that of your homocysteine level, which can be an important root cause factor for the inflammation that can drive both migraine and Alzheimer’s dementia.
You can find a more detailed review at my blog post FAQ Episode 39: Is there a relationship between Migraine and Alzheimer's type dementia?. Also review Question 8 earlier in this interview.
11. You discuss the overlap between fibromyalgia and migraines. What are some common elements in the origin and treatment of these conditions?
One of my blog articles summarizes in greater detail my thoughts on this question and five key overlapping factors for these disorders that I’ll mention below. You can review it at FAQ Episode 49: Fibromyalgia and migraine: are there common elements in origin and treatment?
To respond briefly, as if one ever could on a topic of this breadth and complexity, I find it interesting to consider that both migraine and fibromyalgia:
are far more common in women than men
typically make their appearance during the reproductive years and are often clearly affected by hormonal deficit or imbalance.
have a disturbance of pain and pain perception as a key symptom.
tend to have sleep disruption as either a result of the problem or as a promoting factor and more often, both.
I like to address five areas of perpetuating factors and potential interventions that these two problems have in common:
1) a lack of deep restorative sleep, which is critical for both brain and connective tissue repair, especially with overnight remediation.
It’s pretty safe to predict that the average women with either fibromyalgia, migraine, or worse yet…both, has a problem getting quality sleep. I’ve found that a common element related to deep sleep neuro and muscle repair in both disorders is a deficit in progesterone, testosterone or both. This becomes an even greater concern through the 30s and into the perimenopausal years. Individualized daily or cycle specific hormone support can be a particularly useful benefit in both groups of patients.
2) suboptimal level or imbalance of female reproductive hormones.
For those with heat exchange issues, migraines, or fibromyalgia as they approach menopause, individualized estriol and estradiol therapy can make a critical difference by supporting restorative sleep in both fibro and migraine. My Natural Migraine Relief course has four lessons devoted to specifics on the why and how of female hormone therapy for migraine. It is similarly applicable to fibromyalgia.
3) thyroid hormone balance.
These hormones are the metabolic “spark plugs” for every cell in the body, and when they are at suboptimal levels, cells under perform their vital functions. This in turn can result in low-grade cellular dysfunction and diminished repair capacity. Please see my additional comments on thyroid in the previous question #9 of this interview.
One of the first things I do when I see someone with either fibromyalgia or migraines is to check their thyroid levels and consider support therapy to aim for the upper half or third of the normal range. We don’t really know what any given person’s normal is, and many doctors are fine if it’s in the general “normal range,” even if just barely. Sometimes we need a test drive of two to three months of individualized thyroid support therapy for someone with fibro or migraine is useful to find out if a better version of normal helps you to join the “I didn’t know how bad I was until I got better” club.
4) adrenal hormone support.
Your adrenal hormones are a palette of interconnected compounds with a variety of functions. It is interesting to consider that your cholesterol is the structural platform from which are all made. If your cholesterol is elevated, that could be a sign that you are trying to compensate for either underproduction, or overuse of these hormones. This can happen with chronic stress, and during the perimenopausal years when the adrenal works to compensate for declining ovarian output. If this is true, note well that taking statin drugs may be counter-productive for your migraines.
A key adrenal hormone, DHEA, is the most abundant steroid hormone in the body, and one of its benefits is to counter the stress damaging effects of cortisol. Unfortunately, while DHEA drops over the years, stress induced cortisol often does not. I’ll use two strategies to correct this imbalance and augment adrenal function support for the benefit of both migraine and fibromyalgia:
1) daily adrenal adaptogens like rhodiola, eleuthero, schisandra and ashwagandha in a product like Adrenasense, and
2) lab testing for DHEA-sulphate, and support therapy as indicated. As DHEA can be made into estradiol and testosterone, I would do this under monitoring by a health care professional.
5) Gut dysbiosis, which I discuss in this next question.
When we can find and manage common root cause factors for both fibro and migraine, it can be fun to get a little “two for the price of one” action on results.
12. How does gut health, or dysbiosis, play a role in migraine occurrence? What steps can people with migraine take to improve their gut health?
Your gut health plays a critical role in limiting some important sources of inflammation that can provoke the migraine process.
I like to think of the gut lining as a sort of custom’s officer who patrols a border. In truth, while food is in the pipeline we call the gut, what we chew, digest, and then poop out really isn’t in our body yet. Before getting into the bloodstream, nutrients go through several steps. First, they are broken down into basic units. Proteins à animo acids, carbs à glucose, etc. This requires digestive enzymes, bile salts and the assistance of the bacterial microbiome. Second, they are absorbed through tiny portals in the gut wall, which are just big enough for basic nutrients, but not for larger under digested fragments. If there is an imbalance in the gut bacterial microbiome, food may be undigested, or the gaps in the bowel lining may enlarge, allowing into the bloodstream pro-inflammatory elements. These are recognized as “non-self” by the immune system, and antibodies to them are produced. In what is often called a “leaky gut syndrome,” this process of provocation and inflammation becomes self-perpetuating, and a side product to the immune response can be the promotion or aggravation of disease at more distant locations. Autoimmune problems like Hashimoto’s thyroiditis and celiac disease, or conditions like psoriasis and migraine can be aggravated by this gut generated inflammatory process. It is likely that what is often diagnosed as “irritable bowel syndrome” (IBS) is also a version of this condition. IBS can also promote both fermentation based maldigestion, as well as nutrient deficits. Some of these nutrient deficits can be migraine promoting root cause factors of their own.
Gut dysbiosis is a shorthand term for the condition that perpetuates this vicious cycle and for some promote migraines, as well. For patients with migraine, I address four things related to this condition:
1) identify if there is a “leaky gut” condition and ask what foods might be perpetuating the process. I use a Food Sensitivity Panel, which is a blood test for IgG antibody levels to the most common 100 foods we eat (these are not the IgE antibodies of more severe anaphylactic reactions.) It also includes a test for Candida IgG antibody as well. High levels of antibodies tell us what food fragments the 70% of the immune system that surrounds the gut is reacting to. These are foods in that should be limited or eliminated from the diet for a time. My blog article FAQ Episode 20: How do food sensitivities promote migraine headaches? goes into detail on this topic.
2) find out if there is a candida overgrowth condition by looking at its IgG level. If elevated, we can suspect that candida overgrowth can be taking up the “gut real estate” that should be occupied by beneficial bacterial species. A course of herbal or prescription antifungals may be useful at this juncture, and at times pruning the candida is necessary to allow “re-seeding” with beneficial bacterial to be effective.
3) take a range of beneficial bacteria (probiotics) along with the non-digestible fiber (prebiotics) to feed them. We could spend an hour on the logistical variations of this, so I won’t go into detail here. This blog article reviews the fiber component: FAQ Episode 47: Add the fiber, cut the migraines?
4) avoid direct dietary toxins to the GI tract lining. Consider washing pesticides off fruit, avoiding more than two alcoholic drinks per day, and minimize processed and gluten-based carbs that have higher levels of herbicides, like glyphosate.
Patients with migraines often have some version of IBS and/or gut dysbiosis as a root cause factor in their headaches. If in the process they also under absorb key nutrients, its impact is compounded. This makes the inflammation produced by dysbiosis a relatively high yield root cause factor to investigate.
13. Can you tell us about the role of CGRP in migraines and the new treatments targeting this peptide?
In 2018 a new class of migraine drug was introduced, the first of several that inhibit the action of a protein called calcitonin gene-related peptide (CGRP). When CGRP is released, it causes the dilation of blood vessels in the meninges – the layer of tissue protecting the brain. As the blood vessels dilate, they leak water and proteins into the meninges which causes swelling and irritation. This process relays messages to other regions of the brain, including the thalamus which creates the perception of pain that is associated with a migraine. This really is the first “migraine drug” to directly address a key root cause for migraine. In general, roughly 40-50% of migraine patients will get at least 50% relief benefit from the CGRP medication group.
To address the CGRP non-responders, let’s go a step further, and consider that CGRP activates the trigeminovascular pathway, which collects sensory information from your face: from forehead to chin and everything in between. This information is sent to your brain to be processed. Part of the cascade that leads to a migraine involves the nerves in this pathway, which not only mediate sensations like pain, but also blood flow in the head and face. There are other pro-inflammatory factors that activate this pathway, so finding and managing them along with any pharmaceutical blockade of CGRP may be required to optimize response to this class of drugs. I discuss this in more detail in my blog at FAQ Episode 26: Your response to the latest migraine drugs vs. the root causes of your headaches.
14. You emphasize the importance of certain lab tests for migraine sufferers. Could you walk us through the key tests you recommend - like Vitamin D3, homocysteine, thyroid panel, and DHEA levels? What do these tests reveal about a person's health, how do they relate to migraines, and what insights have you gained from interpreting these results over the years?
Part of the challenge of a medical workup for broad categories like “headaches” is the triage process of getting the essentials done, and yet keeping the process focused to minimize time, trouble, and cost to the patient. Once a working diagnosis of migraine is made, I like to ask: “What information allows me to potentially include-in simple and safe interventions that can make a meaningful difference for the affected patient?” The four tests I recommend for everyone with migraines helps to identify those for whom focused nutritional remediation or prescription thyroid support could address a previously neglected intervention.
Evidence for why checking levels can be important was recently presented (June 2024) at American Headache Society meeting where a review of over 3,400 migraine patients for blood levels of Vitamin D, folate, riboflavin and CoEnzyme Q10 showed that 70% were deficient in at least two of the four (see my FAQ #40 Episode for more details.) From this data, I would emphasize three points:
1) without testing, key deficits for some patients WILL go unrecognized.
2) this is part of why those who take one supplement (when they need two or three) will be disappointed in the results. Clapping with one hand = limited results. Well, who woulda thunk?
3) it is also why I have all my patients take four key nutrients right from the onset of care. 1) Vitamin D, as indicated by blood testing 2) riboflavin 3) CoQ102) and 4) magnesium. Sixty percent all Americans are to some degree magnesium deficient, and a healthy level of this mineral plays a strong role in migraine prophylaxis (see my FAQ Episode # 22 for more information.)
I discussed the value of Vitamin D3, homocysteine and thyroid assessments in previous interview questions. The fourth test, for a DHEA level, is a useful indicator of adrenal sufficiency. You could also add testing for pregnenolone, and A.M. and P.M. cortisol level to be more complete.
DHEA and its precursor pregnenolone are key adrenal building blocks for steroid hormones. These hormones are also neurosteroids and can modulate myelination and inflammation in the central nervous system. They also play a significant role in managing anxiety, sleep quality and the repair of connective tissue. These are areas of concomitant collateral damage in those with chronic migraine. The multiple stressors of having recurrent migraines are also a chronic drain on adrenal resources, so this situation can become a vicious cycle. Providing adrenal support in the form of either adrenal adaptogen herbs or direct DHEA or pregnenolone support is an underutilized and sometimes essential factor to clear migraines. The Natural Migraine Relief course has a full lesson (#17) on the adrenal factor in migraines.
To conclude, I would like to add that checking a CoQ10 level can be helpful for some patients to assure that support doses are sufficient for their condition. This is especially true for those who have fibromyalgia, chronic fatigue or who are taking statin drugs. This test may not be readily available from all local labs. You can get a level done direct-to-consumer at Life Extension labs.
15. For readers who want to learn more about your approach to migraine relief, where can they find your blog and course, and how else can they stay in touch with your work?
I usually make a weekly post to my free Substack blog at naturalmigrainerelief.substack.com where I aim to address how intersecting medical and situational factors affect migraines, along with practical remedial measures. Access to my 25-lesson online course Natural Migraine Relief for Women is for paid subscribers at $7/month. The course uses the unique Migraine Action Plan tool to help you assess the potential overlap of your migraine situation with over 60+ health conditions and medical co-morbidities. It will also direct you to which of more than 90 specific non-drug intervention options are most applicable to your migraine story.
I’m also available for guest blog posts or podcasts, send me a line at baker900@gmail.com. I also welcome feedback from readers, especially concerning migraine related topics I can address in my Substack blog’s “Frequently Asked Questions about Natural Migraine Relief” posts. Just post a comment with your thoughts or questions after any blog article.
Unfortunately, an online blog venue doesn’t allow me to offer patient specific advice on personal medical issues. I am in office practice in Northwest Arkansas and can be contacted to schedule in-person consultation at (479) 756-3251.
I appreciate you being here.
If you've found the content interesting, useful and maybe even helpful, please consider supporting it through a small paid subscription. While everything here is free, your paid subscription is important as it helps in covering some of the operational costs and supports the continuation of this independent research and journalism work. It also helps keep it free for those that cannot afford to pay.
Please make full use of the Free Libraries.
Unbekoming Interview Library: Great interviews across a spectrum of important topics.
Unbekoming Book Summary Library: Concise summaries of important books.
Stories
I'm always in search of good stories, people with valuable expertise and helpful books. Please don't hesitate to get in touch at unbekoming@outlook.com
For COVID vaccine injury
Consider the FLCCC Post-Vaccine Treatment as a resource.
Baseline Human Health
Watch and share this profound 21-minute video to understand and appreciate what health looks like without vaccination.




Many Migraine and Cluster headaches are stopped by Vitamin D, Magnesium, Omega-3, Zinc, etc.
44 studies at https://vitamindwiki.com/tiki-index.php?page_id=3437
Lifelong migraine sufferer.
Headaches are only one part of my symptoms and often not the worst.
Too often people conflate headache with migraine as he says...
Migraines can present without headache.
For some people it can be visual disturbances, vertigo, abdominal pain, and a whole slew of other neurological symptoms...
One question I would have is what to do if two common migraine therapies, vitamin D and riboflavin both give me headache?
I have had more luck with fish oil...