Big Pharma has spent $300 million targeting amyloid, to no avail, and are still mystified by the disease. Both your efforts [Dennis Crouse] and Dr. Bredesen’s book: “The end of Alzheimer’s” brings new hope to cure this terrible disease that robs us of our memories, which is all we really are! – Geoffrey Newton
Dr. Bredesen - he's the first that I have ever heard of to actually reverse neurodegeneration with lifestyle changes such as nutrition. – Roman Shapoval
I’ve produced three stacks so far that cover Alzheimer’s:
In so doing, Dale Bredesen’s name and book kept coming up.
I thought it time to summarize and review it.
Alzheimer’s can be prevented and reversed. There is ample evidence that this is true.
With thanks to Dale Bredesen.
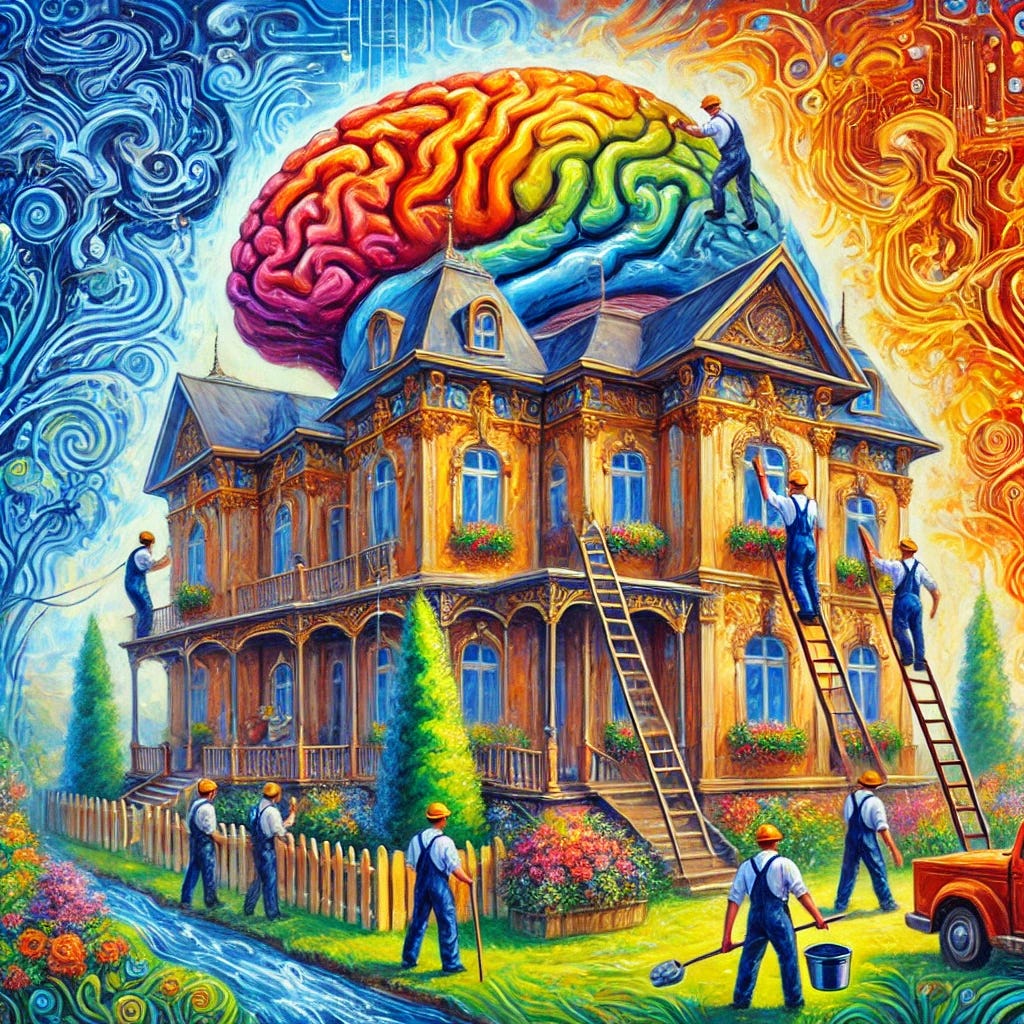
Let’s start with an analogy.
Analogy
Imagine your brain is like a beautiful, complex house. For years, medical experts have been telling us that this house inevitably falls apart as we age, and there's nothing we can do about it. They've focused all their efforts on trying to fix one specific problem - let's say, a leaky roof - thinking that if they could just patch that one hole, the whole house would be saved.
But what I've discovered is that cognitive decline, including Alzheimer's disease, isn't just about one leaky spot. It's more like a house with multiple issues - faulty wiring, clogged pipes, a cracked foundation, and yes, that leaky roof too. Each of these problems represents a different factor contributing to cognitive decline, such as inflammation, hormonal imbalances, toxic exposures, or nutrient deficiencies.
The central message of this book is that to truly protect and restore your brain, you need to address all of these issues simultaneously. It's not enough to just patch the roof if the foundation is still cracking. You need a comprehensive approach that looks at the entire house - or in this case, your whole body and lifestyle - to create an environment where your brain can thrive.
The good news is that, contrary to popular belief, it's possible to not only prevent the house from falling apart but even to renovate and improve it. With the right approach - what I call the ReCODE protocol - we can identify the specific issues affecting your brain-house and address each one. This might involve changes to your diet, exercise routine, sleep habits, stress management, and more, all personalized to your unique needs.
Just as a well-maintained house can last for generations, a well-cared-for brain can remain sharp and functional well into old age. The key is to start taking care of your brain-house early, addressing small issues before they become big problems, and creating an environment that supports cognitive health at every level.
12-point summary
Here's a 12-point summary of the book for those that don’t want to read the deep dive Q&A summary:
Alzheimer's disease is not inevitable or irreversible. It's the result of an imbalance between synapse-creating and synapse-destroying processes in the brain.
There are three main subtypes of Alzheimer's: inflammatory (Type 1), atrophic (Type 2), and toxic (Type 3), each with different underlying causes and requiring different treatment approaches.
The ApoE4 gene is the strongest genetic risk factor for Alzheimer's. Having one copy increases lifetime risk to about 30%, while two copies push it over 50%.
Conventional Alzheimer's treatments have a 99.6% failure rate in clinical trials, highlighting the need for a new approach.
The ReCODE protocol is a personalized, comprehensive approach that has shown success in reversing cognitive decline, even in patients with documented early Alzheimer's.
Key components of the protocol include the "Ketoflex 12/3" diet, regular exercise, stress reduction, quality sleep, brain training, and targeted supplements.
Fasting for at least 12 hours between dinner and breakfast, and for 3 hours before bedtime, can promote brain health through mild ketosis and autophagy.
Chronic inflammation, insulin resistance, and exposure to toxins are major contributors to cognitive decline that need to be addressed.
Optimizing hormone levels, particularly thyroid, sex hormones, and cortisol, is crucial for brain health.
The protocol recommends extensive testing to identify individual risk factors, with patients often showing 10-25 suboptimal lab values contributing to cognitive decline.
Social networking and support groups, like ApoE4.info, play a crucial role in helping patients implement and stick to the protocol.
Early intervention is key: the protocol has shown a 100% success rate in improving cognitive function for those with subjective cognitive impairment (SCI), emphasizing the importance of addressing cognitive health before symptoms become severe.
The End of Alzheimer’s
The First Program to Prevent and Reverse Cognitive Decline
By Dale Bredesen
The End of Alzheimer's: The First... book by Dale Bredesen (thriftbooks.com)
[Unbekoming: The answers are written in the first person, narrated from Dr. Dale Bredesen’s perspective, based solely on the contents of his book.]
45 Questions & Answers
Question 1: What is Alzheimer's disease and how does it differ from normal aging?
Alzheimer's disease is not just a more severe form of normal aging. It's a devastating condition that robs people of their memories, their ability to think clearly, and ultimately their very identity. Unlike normal aging, where some mild forgetfulness might occur, Alzheimer's involves a progressive decline in cognitive abilities that interferes with daily life. It's marked by the formation of amyloid plaques and neurofibrillary tangles in the brain, leading to widespread synaptic loss and neuron death.
The key difference is that Alzheimer's is not an inevitable part of aging. It's a disease process that we now understand is driven by specific factors like inflammation, insulin resistance, and exposure to toxins. This means that, contrary to popular belief, Alzheimer's can potentially be prevented and even reversed in its early stages with the right approach.
Question 2: What are the main signs and stages of cognitive decline?
Cognitive decline typically progresses through several stages, starting with subjective cognitive impairment (SCI), where a person notices subtle changes in their memory or thinking abilities that aren't detectable on standard tests. This can last for a decade or more. The next stage is mild cognitive impairment (MCI), where cognitive deficits become more noticeable and can be measured on tests, but daily functioning isn't significantly impaired.
As the condition progresses to early Alzheimer's disease, symptoms become more pronounced. People may struggle with short-term memory, have difficulty finding words, get lost in familiar places, and have trouble with complex tasks like managing finances. In later stages, long-term memories fade, personality changes occur, and eventually, basic functions like eating and personal care become challenging. It's crucial to recognize and address these changes as early as possible for the best chance of reversal.
Question 3: What is the ReCODE protocol and how was it developed?
The ReCODE (Reversal of Cognitive Decline) protocol is a comprehensive, personalized approach to preventing and reversing cognitive decline, including Alzheimer's disease. It was developed based on three decades of research into the underlying mechanisms of neurodegeneration. The protocol addresses the multiple factors that contribute to cognitive decline, including inflammation, insulin resistance, nutrient and hormone deficiencies, toxin exposure, and more.
ReCODE isn't a one-size-fits-all solution. Instead, it involves a detailed evaluation of each individual's risk factors and biochemistry, followed by a tailored program of interventions. These may include dietary changes, exercise, stress reduction, sleep optimization, targeted supplements, and more. The protocol was refined through years of clinical experience, showing that by addressing the root causes of cognitive decline, it's possible to not just slow the progression of Alzheimer's, but in many cases, reverse it.
Question 4: Who is Dr. Dale Bredesen and what is his background in Alzheimer's research?
I am a neurologist and neuroscientist who has spent over 30 years studying the mechanisms of neurodegenerative diseases, particularly Alzheimer's. My background includes faculty positions at UCSF, UCLA, and UCSD, as well as serving as the founding president and CEO of the Buck Institute for Research on Aging. Throughout my career, I've been driven by a desire to understand why our brains can be so exquisitely productive in youth, yet so vulnerable to decline with age.
My research has led me to challenge the prevailing view of Alzheimer's as an irreversible death sentence for neurons. Instead, I've come to see it as the result of an imbalance in the brain's natural plasticity, triggered by various metabolic and toxic insults. This understanding formed the basis for the development of the ReCODE protocol, which aims to address these underlying causes and restore cognitive function.
Question 5: What is the amyloid hypothesis and why has it been challenged?
The amyloid hypothesis has been the dominant theory in Alzheimer's research for decades. It posits that the accumulation of amyloid-beta protein in the brain is the primary cause of Alzheimer's disease. This led to a focus on developing drugs to remove or prevent the formation of amyloid plaques. However, despite billions of dollars invested in research and numerous clinical trials, this approach has failed to produce effective treatments.
The challenge to this hypothesis comes from mounting evidence that amyloid-beta is actually part of a protective response by the brain to various insults, including inflammation, nutrient deficiencies, and toxin exposure. Amyloid isn't the cause of Alzheimer's, but rather a symptom of these underlying problems. This explains why simply removing amyloid hasn't been effective in treating the disease. Instead, we need to address the factors that are causing the brain to produce amyloid in the first place.
Question 6: How does synaptic loss contribute to Alzheimer's disease progression?
Synaptic loss is at the heart of Alzheimer's disease progression. Synapses are the connections between neurons that allow them to communicate and form memories. In Alzheimer's, there's an imbalance between the processes that create and maintain synapses (synaptoblastic) and those that prune or destroy them (synaptoclastic). This imbalance leads to a net loss of synapses, which correlates strongly with cognitive decline.
The loss of synapses occurs long before neurons themselves die, and it's a key factor in the early symptoms of memory loss and cognitive impairment. As the disease progresses, more and more synapses are lost, leading to widespread dysfunction in the brain's neural networks. Understanding this process is crucial because it means that if we can shift the balance back towards synapse preservation and creation, we have the potential to halt or even reverse cognitive decline.
Question 7: What is the ApoE4 gene and how does it increase Alzheimer's risk?
The ApoE4 gene is the strongest known genetic risk factor for late-onset Alzheimer's disease. It's a variant of the ApoE gene, which comes in three forms: E2, E3, and E4. Everyone inherits two copies of this gene, one from each parent. Having one copy of E4 increases your lifetime risk of Alzheimer's to about 30%, while having two copies pushes it to over 50%.
ApoE4 increases Alzheimer's risk in several ways. It promotes inflammation, reduces the clearance of amyloid-beta from the brain, and affects the production of important brain-supporting molecules. Interestingly, ApoE4 was actually the original form of this gene in humans, and it likely provided advantages in our evolutionary past. However, in our modern environment with longer lifespans and different dietary and lifestyle factors, it has become a liability. The good news is that even if you carry ApoE4, your genes are not your destiny. With the right interventions, you can significantly reduce your risk.
Question 8: How does inflammation contribute to cognitive decline?
Inflammation plays a central role in cognitive decline and Alzheimer's disease. It's one of the three main "threats" that trigger the brain's protective response, which includes the production of amyloid-beta. Chronic inflammation can come from various sources, including infections, poor diet, stress, and environmental toxins. When inflammation persists, it damages neurons and synapses, disrupts the blood-brain barrier, and interferes with normal brain function.
Moreover, inflammation creates a vicious cycle in the brain. It leads to the production of more amyloid-beta, which in turn triggers more inflammation. This chronic state of inflammation also impairs the brain's ability to clear out cellular debris and toxic proteins, further contributing to cognitive decline. By addressing the sources of inflammation and providing anti-inflammatory support, we can help break this cycle and create an environment more conducive to cognitive health.
Question 9: What is the connection between insulin resistance and Alzheimer's disease?
Insulin resistance is so closely linked to Alzheimer's disease that some researchers have dubbed Alzheimer's "type 3 diabetes." When cells become resistant to insulin, it affects their ability to use glucose for energy. This is particularly problematic for brain cells, which have high energy demands. Insulin resistance also interferes with insulin's important role in supporting synapses and neural connections.
Furthermore, chronically high insulin levels have another detrimental effect. The enzyme that degrades insulin, insulin-degrading enzyme (IDE), also degrades amyloid-beta. When IDE is constantly occupied with breaking down excess insulin, it can't effectively clear amyloid-beta from the brain. This leads to an accumulation of amyloid and contributes to the development of Alzheimer's. Addressing insulin resistance through diet, exercise, and other interventions is therefore a crucial part of preventing and treating cognitive decline.
Question 10: How do hormonal imbalances affect cognitive health?
Hormonal balance is crucial for optimal brain function. Many hormones, including estrogen, testosterone, thyroid hormones, and cortisol, play important roles in supporting neuronal health, synaptic function, and cognitive processes. When these hormones are out of balance, it can significantly impact brain health and increase the risk of cognitive decline.
For example, estrogen helps protect neurons and promotes synaptic plasticity. Its decline during menopause is one reason why women are at higher risk for Alzheimer's. Thyroid hormones are essential for brain metabolism and neurotransmitter production. Cortisol, while necessary in the right amounts, can damage the hippocampus when chronically elevated due to stress. Optimizing hormone levels through lifestyle changes and, when necessary, bioidentical hormone replacement therapy, can be an important part of maintaining cognitive health and reversing decline.
Question 11: What types of toxins can impact brain health and how?
There are numerous toxins that can negatively impact brain health, including heavy metals like mercury, lead, and arsenic, as well as biotoxins produced by molds and other microorganisms. These toxins can damage neurons directly, disrupt cellular processes, and trigger inflammation in the brain. For instance, mercury can induce the formation of amyloid plaques and neurofibrillary tangles, hallmarks of Alzheimer's disease.
Another significant source of toxins is our modern environment. Pesticides, air pollution, and even some common household products can contain neurotoxic compounds. Chronic exposure to these toxins can overwhelm the brain's natural detoxification processes, leading to accumulation and damage over time. Identifying and reducing exposure to these toxins, while supporting the body's detoxification pathways, is a crucial part of the ReCODE protocol for preventing and reversing cognitive decline.
Question 12: How does a ketogenic diet potentially benefit brain health?
A ketogenic diet, which is high in healthy fats and low in carbohydrates, can offer several benefits for brain health. When carbohydrate intake is very low, the body shifts from using glucose as its primary fuel to using ketones, which are produced from fat. The brain can efficiently use ketones for energy, and this metabolic state, known as ketosis, has been shown to have neuroprotective effects.
Ketosis helps reduce inflammation, improve insulin sensitivity, and increase the production of brain-derived neurotrophic factor (BDNF), which supports the growth and maintenance of neurons. It also helps starve cancer cells and may reduce the production of amyloid-beta. However, it's important to note that the ketogenic diet in the ReCODE protocol is not the classic very high-fat diet used for epilepsy, but rather a more balanced approach that I call "Ketoflex 12/3," which combines mild ketosis with metabolic flexibility and time-restricted eating.
Question 13: What is the role of fasting in cognitive function?
Fasting plays a crucial role in cognitive function and is a key component of the ReCODE protocol. Specifically, I recommend a practice called "Ketoflex 12/3," where you fast for at least 12 hours between dinner and breakfast (or your first meal the next day), and for at least 3 hours between dinner and bedtime. This fasting period allows your body to enter a state of mild ketosis, which, as mentioned earlier, can have neuroprotective effects.
Fasting also triggers a process called autophagy, where cells recycle damaged components and destroy misfolded proteins. This is particularly important in the brain, as it helps clear out potential neurotoxic substances like amyloid-beta. Additionally, fasting has been shown to increase BDNF levels, improve insulin sensitivity, and reduce inflammation. All of these effects contribute to better cognitive function and can help prevent or reverse cognitive decline.
Question 14: Why is quality sleep crucial for brain health?
Quality sleep is absolutely essential for brain health, and poor sleep is a significant risk factor for cognitive decline and Alzheimer's disease. During sleep, especially the deep stages, the brain undergoes a sort of 'cleaning' process. The space between brain cells expands, allowing for greater flow of cerebrospinal fluid which helps flush out toxins and metabolic waste products, including amyloid-beta.
Sleep is also crucial for memory consolidation, the process by which short-term memories are transferred into long-term storage. Additionally, adequate sleep helps regulate inflammation, improve insulin sensitivity, and maintain hormonal balance. Chronic sleep deprivation, on the other hand, can lead to increased amyloid-beta production, impaired cognitive function, and accelerated brain aging. That's why optimizing sleep duration and quality is a key part of the ReCODE protocol.
Question 15: How does regular exercise impact cognitive function?
Regular exercise is one of the most powerful tools we have for maintaining and improving cognitive function. It benefits the brain in multiple ways. First, it increases blood flow to the brain, delivering more oxygen and nutrients to brain cells. This improved circulation can help support the growth of new blood vessels in the brain, a process called angiogenesis.
Exercise also stimulates the production of BDNF, which promotes the growth and survival of neurons. It helps reduce inflammation, improve insulin sensitivity, and enhance the brain's ability to form new synapses, a process known as neuroplasticity. Furthermore, exercise has been shown to increase the size of the hippocampus, a key region for memory that often shrinks in Alzheimer's disease. For these reasons, I recommend a combination of aerobic exercise and strength training as part of the ReCODE protocol.
Question 16: What stress reduction techniques are recommended for brain health?
Chronic stress can be incredibly damaging to the brain, leading to inflammation, hormonal imbalances, and even shrinkage of key brain areas like the hippocampus. Therefore, stress reduction is a crucial component of the ReCODE protocol. I recommend a variety of techniques, as different approaches work best for different people.
Meditation is one of the most powerful stress-reduction tools. It's been shown to reduce cortisol levels, decrease inflammation, and even increase gray matter volume in the brain. Other effective techniques include deep breathing exercises, yoga, and spending time in nature. Regular exercise, as mentioned earlier, is also a great stress-buster. Additionally, practices like gratitude journaling, listening to music, or engaging in enjoyable hobbies can all help reduce stress levels. The key is to find what works for you and make it a regular part of your routine.
Question 17: What types of brain training exercises can help maintain cognitive function?
Brain training exercises can be valuable tools for maintaining and improving cognitive function. These exercises work by challenging different aspects of cognition, promoting neuroplasticity, and building cognitive reserve. In the ReCODE protocol, I recommend using established brain training programs like BrainHQ, developed by Dr. Michael Merzenich, which has been shown in studies to improve cognitive function and even reduce dementia risk.
Effective brain training should target multiple cognitive domains, including memory, attention, processing speed, and executive function. This might involve tasks like memorizing sequences, solving puzzles, or quickly identifying patterns. However, it's important to note that brain training is most effective when combined with other lifestyle interventions like proper nutrition, exercise, and stress reduction. It's also crucial to continually challenge yourself with new and progressively difficult tasks to keep your brain engaged and growing.
Question 18: Which supplements are suggested for cognitive health in the ReCODE protocol?
The ReCODE protocol includes a variety of supplements tailored to each individual's needs based on their lab results. However, some key supplements that are often recommended include:
Omega-3 fatty acids (DHA and EPA) for their anti-inflammatory and neuroprotective effects.
B vitamins, particularly B12, folate, and B6, to help lower homocysteine levels.
Vitamin D3 with K2, as many people are deficient and it plays crucial roles in brain health.
Turmeric (curcumin) for its potent anti-inflammatory effects.
Probiotics and prebiotics to support gut health, which is closely linked to brain health.
Other supplements might include resveratrol, coenzyme Q10, alpha-lipoic acid, and specific herbal supplements like bacopa and ashwagandha. However, it's important to note that supplements should be used as part of a comprehensive approach, not as a standalone solution, and should be tailored to each individual's needs based on thorough testing.
Question 19: How does a personalized medicine approach differ from traditional Alzheimer's treatment?
The personalized medicine approach of the ReCODE protocol differs dramatically from traditional Alzheimer's treatment. Conventional medicine typically relies on a one-size-fits-all approach, often focusing on a single drug designed to address a single aspect of the disease, such as breaking down amyloid plaques. This approach has consistently failed in clinical trials.
In contrast, the ReCODE protocol recognizes that Alzheimer's is a complex, multifactorial disease that can have different underlying causes in different individuals. We use extensive testing to identify each person's specific risk factors and metabolic imbalances. Then, we create a personalized treatment plan that addresses all of these factors simultaneously. This might involve dietary changes, exercise, stress reduction, sleep optimization, targeted supplements, and more. The goal is to address the root causes of cognitive decline, not just treat the symptoms. This personalized, comprehensive approach has shown far greater success in preventing and reversing cognitive decline than traditional treatments.
Question 20: What is the connection between gut health and cognitive function?
The connection between gut health and cognitive function is a fascinating and rapidly growing area of research. We now know that there's a bi-directional communication system between the gut and the brain, often referred to as the gut-brain axis. The health of your gut microbiome - the trillions of bacteria that live in your digestive system - can significantly impact your brain health and cognitive function.
A healthy gut microbiome helps maintain the integrity of the intestinal lining, preventing "leaky gut" which can lead to systemic inflammation - a key driver of cognitive decline. Certain gut bacteria also produce neurotransmitters and other compounds that can influence brain function. Moreover, the gut is intimately connected to the immune system, and gut dysbiosis (an imbalance in gut bacteria) can lead to chronic inflammation that affects the brain. That's why the ReCODE protocol includes strategies to optimize gut health, including dietary changes, stress reduction, and the use of probiotics and prebiotics when appropriate.
Question 21: What are the three main types of Alzheimer's disease described in the book?
In my research, I've identified three main subtypes of Alzheimer's disease, each with distinct underlying causes and characteristics:
Type 1 (Inflammatory): This type is associated with systemic inflammation, often related to factors like insulin resistance, metabolic syndrome, or chronic infections. It typically affects ApoE4 carriers and presents with symptoms like losing the ability to form new memories.
Type 2 (Atrophic): This subtype is characterized by a lack of trophic support - essentially, the brain isn't getting enough of the nutrients and growth factors it needs to maintain synapses. It's often associated with hormonal imbalances, nutrient deficiencies, and insulin resistance.
Type 3 (Toxic): This is the most difficult type to treat and often occurs in people without the ApoE4 gene. It's caused by exposure to specific toxins, such as heavy metals or biotoxins from mold. Symptoms often start with non-memory problems like difficulty calculating or finding words.
Understanding these subtypes is crucial because each requires a different treatment approach. Many patients have a combination of these subtypes, which is why a personalized, comprehensive treatment plan is so important.
Question 22: What biomarkers are used to assess Alzheimer's risk?
Assessing Alzheimer's risk involves looking at a wide range of biomarkers, far beyond what's typically checked in standard medical exams. Some key biomarkers we look at include:
Inflammatory markers like hs-CRP, IL-6, and TNF-alpha
Metabolic markers such as fasting insulin, hemoglobin A1c, and fasting glucose
Hormonal levels, including thyroid hormones, sex hormones, and cortisol
Nutrient levels, particularly vitamins B12, D, and E
Toxin levels, including heavy metals and mycotoxins
Genetic factors, especially ApoE status
Homocysteine levels
Lipid profiles, including LDL particle number and size
We also look at markers of gut health, immune function, and oxidative stress. The goal is to get a comprehensive picture of a person's metabolic status and identify all potential contributors to cognitive decline. This allows us to create a targeted, personalized treatment plan.
Question 23: How do neuroimaging techniques contribute to Alzheimer's diagnosis and research?
Neuroimaging techniques have revolutionized our ability to diagnose Alzheimer's disease and understand its progression. Some key imaging methods include:
MRI (Magnetic Resonance Imaging): This can show brain atrophy, particularly in the hippocampus, which is often one of the first areas affected in Alzheimer's. Advanced MRI techniques can also reveal changes in brain connectivity.
PET (Positron Emission Tomography): Amyloid PET scans can detect the presence of amyloid plaques in the living brain, while FDG-PET scans can show patterns of decreased glucose metabolism characteristic of Alzheimer's.
SPECT (Single Photon Emission Computed Tomography): This can reveal blood flow patterns in the brain, which are often altered in Alzheimer's.
These imaging techniques allow us to detect brain changes associated with Alzheimer's before symptoms become apparent, enabling earlier intervention. They're also valuable research tools, helping us understand how the disease progresses and how different treatments affect the brain. However, it's important to note that imaging should always be interpreted in the context of a person's overall clinical picture and other biomarkers.
Question 24: What key patient stories and case studies are presented in the book?
Throughout the book, I share several patient stories that illustrate the effectiveness of the ReCODE protocol. One key case is that of Patient Zero, a 67-year-old woman who was experiencing severe cognitive decline and was preparing to resign from her job. After starting the protocol, she showed significant improvement within three months and has maintained her cognitive health for years.
Another striking case is that of a 69-year-old entrepreneur with well-documented early Alzheimer's disease. He had been told to get his affairs in order, but after following the protocol, he was able to return to work, expand his business, and show dramatic improvement on cognitive tests.
I also discuss cases of patients with different subtypes of Alzheimer's, including a woman with toxic (Type 3) Alzheimer's who improved after addressing mold exposure, and several patients with the inflammatory (Type 1) subtype who showed reversal of cognitive decline after addressing metabolic issues.
These case studies demonstrate that cognitive decline can be reversed, even in cases of documented Alzheimer's disease, when all contributing factors are comprehensively addressed.
Question 25: What criticisms and resistance has the ReCODE approach faced?
The ReCODE approach has faced several criticisms and encountered resistance from the medical establishment. Some common objections include:
Skepticism about the possibility of reversing cognitive decline, given the long-held belief that Alzheimer's is irreversible.
Concerns about the complexity of the protocol, with some arguing it's too complicated for widespread adoption.
Criticism that the approach hasn't been validated in large, randomized controlled trials.
Resistance to the idea that Alzheimer's could have multiple subtypes requiring different treatment approaches.
Skepticism from those invested in the amyloid hypothesis and drug development based on this theory.
Many of these criticisms stem from the paradigm shift that ReCODE represents. It challenges the traditional single-drug approach to treating Alzheimer's and requires a more comprehensive understanding of the disease's underlying mechanisms. Despite these challenges, the growing number of success stories and the increasing recognition of the role of lifestyle factors in cognitive health are gradually shifting perspectives.
Question 26: How can social networking benefit Alzheimer's patients and their families?
Social networking can be immensely beneficial for Alzheimer's patients and their families in several ways:
Support and Understanding: Connecting with others going through similar experiences can provide emotional support and reduce feelings of isolation.
Information Sharing: Social networks allow patients and families to share information about treatments, coping strategies, and the latest research.
Motivation and Accountability: Being part of a community can help patients stay motivated to follow their treatment protocols and make lifestyle changes.
Collective Problem-Solving: Groups can pool their experiences to find solutions to common challenges faced in managing the disease.
Advocacy: Social networks can be powerful tools for raising awareness and advocating for better research and treatment options.
A prime example is the ApoE4.info website, created by ReCODE patients. This platform has become a valuable resource for information sharing, support, and collaborative problem-solving among individuals at risk for or dealing with Alzheimer's disease. Such networks play a crucial role in empowering patients and families to take an active role in managing cognitive health.
Question 27: What lifestyle changes are recommended for preventing and reversing cognitive decline?
The ReCODE protocol recommends a comprehensive set of lifestyle changes to prevent and reverse cognitive decline:
Diet: Adopt a "Ketoflex 12/3" diet, which is a flexible, mildly ketogenic diet with an emphasis on plant-based foods and healthy fats. This includes a 12-hour fasting period overnight and at least a 3-hour gap between dinner and bedtime.
Exercise: Engage in regular physical activity, including both aerobic exercise and strength training, for at least 45 minutes per day, 4-6 days per week.
Sleep: Prioritize getting 7-8 hours of quality sleep each night. Address any sleep disorders like sleep apnea.
Stress Reduction: Practice stress-reduction techniques such as meditation, yoga, or deep-breathing exercises.
Brain Training: Engage in cognitive stimulation activities and brain training exercises regularly.
Social Engagement: Maintain strong social connections and engage in meaningful activities.
Toxin Avoidance: Minimize exposure to environmental toxins and support the body's detoxification processes.
Hormone Optimization: Work with a healthcare provider to optimize hormone levels if necessary.
These lifestyle changes work synergistically to create an environment in the body and brain that supports cognitive health and resilience against neurodegenerative processes.
Question 28: What is the current state of mainstream Alzheimer's research and treatment?
The current state of mainstream Alzheimer's research and treatment is, frankly, disappointing. Despite billions of dollars invested in research and hundreds of clinical trials, we still have no effective treatment to stop or reverse the progression of Alzheimer's disease. The primary focus has been on developing drugs to target amyloid plaques, based on the amyloid hypothesis. However, these efforts have consistently failed in clinical trials.
The standard of care for Alzheimer's patients typically involves drugs like cholinesterase inhibitors (e.g., donepezil) or memantine, which may temporarily improve symptoms but do not alter the course of the disease. Many physicians still tell patients that there's nothing they can do to prevent or reverse cognitive decline.
This state of affairs underscores the need for a paradigm shift in how we approach Alzheimer's disease. We need to move beyond the single-target, single-drug approach and embrace a more comprehensive understanding of the disease's multiple underlying causes. This is where approaches like ReCODE, which address multiple factors simultaneously, offer new hope.
Question 29: How might Alzheimer's prevention and treatment evolve in the future?
The future of Alzheimer's prevention and treatment is likely to be characterized by several key trends:
Personalized Medicine: Treatment will become increasingly tailored to individual patients based on their unique genetic, metabolic, and environmental risk factors.
Early Intervention: There will be a greater emphasis on identifying and addressing risk factors decades before symptoms appear.
Comprehensive Approaches: Instead of relying on single drugs, treatment will likely involve multi-faceted protocols addressing diet, lifestyle, and targeted interventions.
Advanced Diagnostics: We'll see more sophisticated biomarker testing and imaging techniques to detect early signs of cognitive decline.
Combination Therapies: Even as drug development continues, future treatments may combine pharmaceuticals with lifestyle interventions for better results.
Focus on Prevention: There will be a shift towards preventing Alzheimer's rather than just treating it after symptoms appear.
Increased Use of Technology: Digital health tools, AI, and telemedicine will play larger roles in monitoring cognitive health and delivering interventions.
The key to this evolution will be a deeper understanding of the complex factors contributing to cognitive decline and a willingness to move beyond the traditional drug-centered approach to treatment.
Question 30: Why is early detection and intervention crucial in addressing cognitive decline?
Early detection and intervention are absolutely critical in addressing cognitive decline for several reasons:
Reversibility: The earlier cognitive decline is detected, the more likely it is to be reversible. Once significant brain atrophy has occurred, it becomes much more challenging to restore function.
Preservation of Function: Early intervention can help maintain cognitive abilities and independence for longer, significantly improving quality of life.
Addressing Root Causes: Early detection allows us to identify and address the underlying causes of cognitive decline before they cause irreversible damage.
More Treatment Options: In earlier stages, patients have more treatment options available and are better able to actively participate in their treatment.
Slowing Progression: Even if cognitive decline can't be completely reversed, early intervention can significantly slow its progression.
Cost-Effectiveness: Preventing or reversing cognitive decline early is far more cost-effective than treating advanced Alzheimer's disease.
Time for Lifestyle Changes: Early detection gives individuals time to make the necessary lifestyle changes that can have a significant impact on cognitive health.
This is why I advocate for everyone to get a "cognoscopy" - a thorough evaluation of cognitive health and risk factors - by age 45. The goal is to identify potential issues decades before symptoms appear, when intervention can be most effective.
Question 31: Beyond ApoE4, what other genetic factors influence Alzheimer's risk?
While ApoE4 is the most well-known genetic risk factor for Alzheimer's, there are several other genes that can influence risk:
APP (Amyloid Precursor Protein): Mutations in this gene can lead to early-onset Alzheimer's disease.
PSEN1 and PSEN2 (Presenilin 1 and 2): These genes are also associated with early-onset Alzheimer's.
TREM2: Variants of this gene can increase Alzheimer's risk by affecting the immune system's ability to clear amyloid from the brain.
CLU (Clusterin): This gene is involved in lipid metabolism and has been linked to increased Alzheimer's risk.
PICALM: This gene affects the clearance of amyloid-beta from the brain.
CR1: This gene is involved in the complement system, part of the immune response, and variants can increase Alzheimer's risk.
It's important to note that having these genetic variants doesn't guarantee you'll develop Alzheimer's. They interact with environmental and lifestyle factors to influence risk. Understanding your genetic profile can help inform prevention strategies, but it's just one piece of the puzzle.
Question 32: How does mitochondrial function relate to cognitive health?
Mitochondria, often called the powerhouses of the cell, play a crucial role in cognitive health. They're responsible for producing the energy our brain cells need to function properly. When mitochondrial function declines, it can have significant impacts on cognitive health:
Energy Production: Reduced mitochondrial function means less energy for brain cells, impairing their ability to form and maintain synapses.
Oxidative Stress: Dysfunctional mitochondria produce more free radicals, leading to oxidative stress and cellular damage.
Apoptosis: Mitochondria play a key role in programmed cell death. Dysfunction can lead to inappropriate neuron loss.
Calcium Regulation: Mitochondria help regulate calcium levels in neurons, which is crucial for synaptic function.
Neuroplasticity: Optimal mitochondrial function is necessary for the brain's ability to form new neural connections.
In Alzheimer's disease, mitochondrial dysfunction is often observed early in the disease process. Supporting mitochondrial health through diet, exercise, and targeted supplements is an important part of the ReCODE protocol.
Question 33: Why is detoxification important for brain health?
Detoxification is crucial for brain health because our modern environment exposes us to a multitude of toxins that can damage brain cells and contribute to cognitive decline. These toxins include heavy metals, pesticides, air pollutants, and biotoxins from molds and other microorganisms.
The brain has its own detoxification system, including the glymphatic system, which clears out metabolic waste products during sleep. However, this system can become overwhelmed by chronic toxin exposure. Accumulated toxins can cause inflammation, oxidative stress, and direct damage to neurons and synapses.
Supporting the body's detoxification processes can help reduce this toxic burden. This includes optimizing liver function, supporting kidney health, ensuring adequate hydration, and promoting healthy elimination through the digestive system. Specific detox-supporting nutrients and practices, such as glutathione supplementation and sauna use, can also be beneficial.
In the ReCODE protocol, we assess each individual's toxic burden and tailor detoxification strategies accordingly. This is particularly important for those with Type 3 (toxic) Alzheimer's, where toxin exposure plays a central role in cognitive decline.
Question 34: What environmental factors can contribute to cognitive decline?
Environmental factors play a significant role in cognitive health and can contribute to cognitive decline in various ways:
Air Pollution: Exposure to fine particulate matter and other air pollutants has been linked to increased risk of cognitive decline and dementia.
Heavy Metals: Chronic exposure to metals like mercury, lead, and arsenic can be neurotoxic.
Pesticides: Some pesticides have been associated with increased risk of neurodegenerative diseases.
Mold and Mycotoxins: Exposure to toxic mold in buildings can contribute to cognitive issues, particularly in susceptible individuals.
Electromagnetic Fields (EMFs): While controversial, some research suggests that long-term EMF exposure may affect brain function.
Noise Pollution: Chronic exposure to high noise levels can increase stress and potentially impact cognitive function.
Lack of Nature Exposure: Limited access to natural environments may negatively affect mental health and cognitive function.
Poor Indoor Air Quality: Inadequate ventilation and exposure to indoor pollutants can affect brain health.
Recognizing these environmental factors is crucial because many are modifiable. The ReCODE protocol includes strategies to reduce exposure to harmful environmental factors and support the body's ability to deal with unavoidable exposures.
Question 35: What is the blood-brain barrier and how does it relate to Alzheimer's disease?
The blood-brain barrier is a highly selective semipermeable border of endothelial cells that prevents substances in the bloodstream from freely passing into the extracellular fluid of the central nervous system where neurons reside. It's crucial for maintaining a stable environment for proper brain function.
In Alzheimer's disease, the integrity of the blood-brain barrier is often compromised. This "leaky" blood-brain barrier can allow harmful substances to enter the brain, including pathogens, toxins, and inflammatory molecules. It can also impair the clearance of amyloid-beta from the brain.
Several factors can contribute to blood-brain barrier dysfunction, including chronic inflammation, high blood sugar levels, and certain infections. Improving blood-brain barrier integrity is an important aspect of the ReCODE protocol. This can be achieved through strategies like reducing inflammation, optimizing blood sugar control, and supporting the production of proteins that maintain the barrier's structure.
Understanding the role of the blood-brain barrier in Alzheimer's disease has opened up new avenues for both prevention and treatment strategies.
Question 36: How does oral health potentially impact cognitive function?
Oral health has a surprisingly significant impact on cognitive function, and poor oral health has been linked to increased risk of cognitive decline and Alzheimer's disease. There are several ways in which oral health affects brain health:
Inflammation: Periodontal disease can lead to chronic systemic inflammation, which is a key driver of cognitive decline.
Bacterial Invasion: Oral bacteria, particularly Porphyromonas gingivalis, have been found in the brains of Alzheimer's patients. These bacteria can potentially cross the blood-brain barrier and contribute to neuroinflammation.
Nutritional Impact: Poor oral health can affect nutrition by limiting the types of foods a person can eat, potentially leading to nutrient deficiencies that impact brain health.
Vascular Effects: The inflammation associated with gum disease can affect blood vessels throughout the body, including those in the brain.
Stress: Chronic oral health issues can be a source of stress, which itself is a risk factor for cognitive decline.
Given these connections, maintaining good oral hygiene and addressing any dental issues promptly is an important part of a comprehensive approach to cognitive health. Regular dental check-ups, proper brushing and flossing, and addressing any infections or inflammation in the mouth are all crucial steps.
Question 37: What specific heavy metals are concerning for brain health and why?
Several heavy metals are particularly concerning for brain health due to their neurotoxic effects:
Mercury: It can cross the blood-brain barrier and cause neuronal damage. Sources include certain fish, dental amalgams, and some industrial processes.
Lead: Even low-level exposure can impair cognitive function. It can accumulate in the brain over time. Sources include old paint, contaminated soil, and some industrial processes.
Aluminum: While not a heavy metal, it's often grouped with them. It's been found in higher concentrations in the brains of Alzheimer's patients. Sources include some cookware, antacids, and antiperspirants.
Arsenic: It can cross the blood-brain barrier and interfere with neurotransmitter function. Sources include contaminated water and some foods.
Cadmium: It can accumulate in the brain and cause oxidative stress. Sources include cigarette smoke and some industrial processes.
These metals can damage neurons directly, promote inflammation, increase oxidative stress, and interfere with important cellular processes in the brain. In the ReCODE protocol, we assess for heavy metal exposure and implement strategies to reduce exposure and support the body's detoxification processes when necessary.
Question 38: How does the sinus microbiome potentially affect cognitive health?
The sinus microbiome, the community of microorganisms living in our nasal passages and sinuses, is emerging as an important factor in cognitive health. This is particularly relevant to what I call Type 3 Alzheimer's disease, which is often associated with toxin exposure and chronic inflammatory response syndrome (CIRS).
Here's how the sinus microbiome can affect cognitive health:
Direct Access to the Brain: The nose provides a direct route to the brain, bypassing the blood-brain barrier. Pathogens or toxins in the sinuses can potentially travel along the olfactory nerve to the brain.
Mycotoxin Production: In some cases, fungi in the sinuses can produce mycotoxins, which are potent neurotoxins that can contribute to cognitive decline.
Chronic Inflammation: An imbalanced sinus microbiome can lead to chronic sinus infections and inflammation, which can have systemic effects including neuroinflammation.
Immune System Activation: Certain microbes in the sinuses can trigger an ongoing immune response that may contribute to neuroinflammation.
Olfactory Function: The health of the sinus microbiome can affect our sense of smell, which is often one of the first senses affected in Alzheimer's disease.
In the ReCODE protocol, we assess the health of the sinus microbiome in patients showing signs of Type 3 Alzheimer's. Treatment may involve addressing any infections, reducing exposure to mold and mycotoxins, and supporting a healthy sinus microbiome.
Question 39: Which hormones are particularly important to optimize for cognitive function?
Several hormones play crucial roles in cognitive function, and optimizing their levels can be an important part of preventing and reversing cognitive decline:
Thyroid Hormones: These regulate metabolism in every cell of the body, including brain cells. Both high and low thyroid function can impair cognition.
Estrogen: It supports synaptic health and has neuroprotective effects. The decline in estrogen during menopause is one reason why women are at higher risk for Alzheimer's.
Testosterone: Important for both men and women, it supports cognitive function and neuroprotection.
Progesterone: It has neuroprotective effects and helps balance estrogen.
Cortisol: While necessary in the right amounts, chronically high cortisol due to stress can damage the hippocampus.
Pregnenolone: This is a precursor to many other hormones and supports cognitive function directly.
DHEA: It has neuroprotective effects and declines with age.
Insulin: Proper insulin function is crucial for brain health. Insulin resistance in the brain is a key feature of Alzheimer's disease.
In the ReCODE protocol, we assess hormone levels and function, and work to optimize them through lifestyle interventions and, when necessary, bioidentical hormone replacement therapy. It's important to note that this should always be done under the guidance of a knowledgeable healthcare provider, as hormone balance is complex and individual.
Question 40: What is neuroplasticity and how does it relate to Alzheimer's treatment?
Neuroplasticity refers to the brain's ability to form new neural connections, reorganize existing ones, and even grow new neurons throughout life. This capacity for change and adaptation is crucial for learning, memory, and recovery from brain injury.
In the context of Alzheimer's treatment, neuroplasticity offers hope for several reasons:
Compensation: Even as some brain areas are damaged, other areas can potentially take over their functions through neuroplasticity.
Repair: The brain can potentially repair some of the damage caused by Alzheimer's by forming new synapses and neural pathways.
Cognitive Reserve: A lifetime of learning and mental stimulation can build up cognitive reserve, which may help the brain compensate for damage and delay symptom onset.
Treatment Response: Interventions that support neuroplasticity, such as cognitive stimulation and certain nutrients, may help slow or reverse cognitive decline.
Resilience: A brain with greater neuroplasticity may be more resilient to the damage caused by Alzheimer's pathology.
The ReCODE protocol aims to support and enhance neuroplasticity through various interventions, including brain training exercises, optimizing nutrition, hormones, and other factors that support brain health. By creating an environment that supports neuroplasticity, we can potentially help the brain resist and recover from the damage associated with Alzheimer's disease.
Question 41: How does functional medicine approach the treatment of cognitive decline?
Functional medicine approaches the treatment of cognitive decline in a fundamentally different way from conventional medicine. Here are the key aspects:
Root Cause Analysis: Instead of just treating symptoms, functional medicine seeks to identify and address the underlying causes of cognitive decline, which can vary from person to person.
Systems Biology Approach: It recognizes that cognitive health is influenced by multiple interconnected systems in the body, including the immune system, gut health, hormonal balance, and more.
Personalization: Treatment plans are highly individualized based on a person's unique genetic, biochemical, and lifestyle factors.
Prevention Focus: There's a strong emphasis on preventing cognitive decline before symptoms appear, rather than just treating it after the fact.
Comprehensive Interventions: Treatment typically involves a combination of dietary changes, targeted supplements, exercise, stress reduction, and other lifestyle modifications.
Ongoing Optimization: Rather than a one-time intervention, functional medicine involves ongoing monitoring and adjustment of the treatment plan.
Patient Empowerment: Patients are seen as active participants in their health, educated about their condition and empowered to make lifestyle changes.
This approach aligns closely with the ReCODE protocol, which is why many functional medicine practitioners have been early adopters of this method for treating cognitive decline.
Question 42: Why is addressing multiple factors simultaneously important in treating Alzheimer's?
Addressing multiple factors simultaneously is crucial in treating Alzheimer's disease for several reasons:
Complex Etiology: Alzheimer's is not caused by a single factor, but by a complex interplay of genetic, environmental, and lifestyle factors. Addressing only one aspect is unlikely to be effective.
Synergistic Effects: Many of the factors contributing to Alzheimer's interact with and amplify each other. Addressing multiple factors can create synergistic benefits.
Individual Variations: Different individuals may have different underlying causes driving their cognitive decline. A multi-factor approach is more likely to address each person's unique situation.
Threshold Effect: There seems to be a threshold that needs to be crossed to shift from cognitive decline to cognitive improvement. Addressing multiple factors increases the likelihood of crossing this threshold.
Holistic Brain Health: Factors like diet, exercise, sleep, and stress affect overall brain health in multiple ways. Optimizing all of these creates a brain-healthy environment.
Resilience: By improving multiple aspects of brain health, we can increase the brain's resilience against further damage.
Feedback Loops: Many factors in Alzheimer's create vicious cycles. Breaking these cycles often requires intervening at multiple points simultaneously.
This is why the ReCODE protocol is designed as a comprehensive program addressing numerous factors, rather than a single intervention. It's akin to patching multiple holes in a leaky roof, rather than just focusing on one.
Question 43: What is metabolic flexibility and why is it important for brain health?
Metabolic flexibility refers to the body's ability to efficiently switch between different fuel sources, primarily glucose and ketones. This ability is crucial for overall health, including brain health, for several reasons:
Energy Efficiency: A metabolically flexible brain can use whatever fuel is most readily available, ensuring a constant energy supply.
Neuroprotection: Ketones, produced when glucose is low, have neuroprotective properties and can help support brain function during metabolic stress.
Insulin Sensitivity: Metabolic flexibility is closely tied to insulin sensitivity, which is important for brain health. Insulin resistance in the brain is a key feature of Alzheimer's disease.
Inflammation Reduction: Switching between fuel sources can help reduce chronic inflammation, a key driver of cognitive decline.
Cellular Clean-up: Periods of lower glucose availability can trigger autophagy, a cellular clean-up process that's important for brain health.
Cognitive Performance: Some studies suggest that the brain functions better when it can efficiently use both glucose and ketones.
The "Ketoflex 12/3" diet in the ReCODE protocol is designed to promote metabolic flexibility. It combines periods of mild ketosis with the ability to use glucose when needed. This approach aims to give the brain the metabolic resilience it needs to resist cognitive decline and support optimal function.
Question 44: What are advanced glycation end products (AGEs) and how do they affect cognitive health?
Advanced glycation end products, or AGEs, are harmful compounds that form when proteins or fats combine with sugars in the bloodstream. This process, called glycation, is a normal part of aging, but it's accelerated by high blood sugar levels and certain cooking methods. AGEs are relevant to cognitive health in several ways:
Inflammation: AGEs trigger inflammation in the body and brain, a key driver of cognitive decline.
Oxidative Stress: They increase oxidative stress, which can damage brain cells and contribute to neurodegeneration.
Amyloid Formation: AGEs can promote the formation and aggregation of amyloid-beta, a hallmark of Alzheimer's disease.
Vascular Damage: They can damage blood vessels, including those in the brain, potentially contributing to vascular dementia.
Insulin Resistance: AGEs interfere with insulin signaling, potentially contributing to brain insulin resistance, a feature of Alzheimer's.
Cross-linking: AGEs can cause proteins to cross-link, interfering with their normal function and potentially contributing to the formation of neurofibrillary tangles.
To reduce AGE formation and accumulation, the ReCODE protocol recommends a diet low in added sugars and processed foods, avoiding high-temperature cooking methods like frying and grilling, and including foods and supplements that may help counteract AGEs, such as certain herbs and spices.
Question 45: How does personalized nutrition factor into the ReCODE protocol?
Personalized nutrition is a cornerstone of the ReCODE protocol, recognizing that dietary needs can vary significantly between individuals based on their genetic makeup, current health status, and specific risk factors for cognitive decline. Here's how personalized nutrition factors into the protocol:
Genetic Considerations: For example, ApoE4 carriers may benefit from a diet higher in certain types of fats compared to non-carriers.
Metabolic Status: The diet is tailored based on factors like insulin sensitivity, inflammation levels, and lipid profiles.
Food Sensitivities: Individual food sensitivities or allergies are identified and addressed to reduce inflammation.
Nutrient Deficiencies: Specific dietary recommendations are made to address any identified nutrient deficiencies.
Gut Health: The diet is designed to support a healthy gut microbiome, which can vary between individuals.
Detoxification Support: Dietary recommendations may be tailored to support the body's detoxification processes based on individual toxic burden.
Ketosis Levels: The level of ketosis recommended may vary based on individual factors and response.
Timing of Meals: The fasting period and meal timing are personalized based on individual metabolic patterns and lifestyle.
This personalized approach ensures that each individual is getting the precise nutritional support they need to optimize their brain health and cognitive function. It's not just about following a one-size-fits-all "brain-healthy diet," but about creating a nutritional plan that addresses each person's unique needs and risk factors.
I appreciate you being here.
If you've found the content interesting, useful and maybe even helpful, please consider supporting it through a small paid subscription. While everything here is free, your paid subscription is important as it helps in covering some of the operational costs and supports the continuation of this independent research and journalism work. It also helps keep it free for those that cannot afford to pay.
Please make full use of the Free Libraries.
Unbekoming Interview Library: Great interviews across a spectrum of important topics.
Unbekoming Book Summary Library: Concise summaries of important books.
Stories
I'm always in search of good stories, people with valuable expertise and helpful books. Please don't hesitate to get in touch at unbekoming@outlook.com
For COVID vaccine injury
Consider the FLCCC Post-Vaccine Treatment as a resource.
Baseline Human Health
Watch and share this profound 21-minute video to understand and appreciate what health looks like without vaccination.




Great post. It's been interesting to see the different theories everyone has about Alzheimer's, but it seems to me that you can't go wrong if you use the lifestyle changes described here, detox for Aluminum and Mercury, and fix leaky gut syndrome. I did all that plus eliminated all vegetable and seed oils when I learned the brain is 75% cholesterol, and added a pinch of sea salt with each glass of water. No more falls or forgetfulness, no more psych meds, feeling like a new person.
Alzheimers is also known as Diabetes type 3