They are not told that their lives will be shorter, that they will suffer more from osteoporosis, that they may never have restorative sleep again, that they will suffer the loss of muscle mass from the lost testosterone, that they will be anxious, enraged, panicky and perhaps diagnosed with a mental illness, that they will be offered a long list of pharmaceuticals for symptom relief which will fail them, that their bodies will suffer with pain and the list goes on.
Carol Petersen
We are going to circle back to where this current Hysterectomy journey started.
Back to Carol Petersen.
In our first interview Carol said:
“Most reasons for hysterectomies can be tied to progesterone deficiencies and most could be avoided with rational supplementation.”
I went back to Carol and asked if she would be open to another interview, this time focused on how woman can address and resolve the symptoms and conditions that conventional medicine typically uses to justify life altering surgery.
I’m grateful that she agreed, and we now have a wonderful conversation that hopefully will help more women make better and more informed choices about what to do with their bodies.
With gratitude, I give you Carol Peterson RPh, CNP.
The Wellness By Design Project
1. Could you share your experience with women who come to you having been recommended a hysterectomy by their doctors? What initial advice do you typically give?
Women who have had a hysterectomy have a long time deficiency with progesterone. They have suffered with PMDD, PMS, PCOS, Infertility, endometriosis, fibroids, very heavy bleeding, cysts on the ovaries, and even uterine cancer. Their doctors remove ovaries along with the uterus quite frequently and then supply women with 1 hormone – an estrogen. The ovaries have supplied estrogens, progesterone, testosterone, DHEA and likely much more. This estrogen supplementation continues to create more sleep problems, anxiety, panic, rage, depression, fatigue, pain, cardiac and blood pressure problems, metabolic syndrome with insulin glucose imbalances. Sadly, it is a rare opportunity to intervene before surgery. The message I’d like to convey here is that it is possible to restore hormones to both correct those presurgical problems AND to restore hormones after surgery to have a reasonable quality of life.
2. How do you approach cases where surgery seems imminent? Can you describe your process for assessing whether alternative treatments might be viable?
Our society minimizes the horror of surgery. The assault to the body for any surgery is massive and has consequences. As I just mentioned, it is a rare occasion that interventions can be made before a surgery. Those women who are facing this prospect have been thoroughly conditioned to believe that this is their only option. Heavy bleeding in perimenopause is a major reason for hysterectomy. Conventional medicine does not intervene until the bleeding is so great that it seems to be life threatening. Yet, it is easily reversed with progesterone supplementation in the follicular phase of the menstrual cycle. As a society, we are preconditioned to consult with conventional medicine doctors for advice and treatment even though they are ignorant of many treatment options.
3. In your practice, how do you use bioidentical hormones to address the symptoms and issues leading to the recommendation of hysterectomy? Can you give an example of how this has prevented surgery for some women?
It is very easy to stop excessive uterine bleeding. During perimenopause, Dr. Jerilyn Prior (cemcor.ca) states that women have the highest estrogen of their life span. This is coupled with increased missed ovulations and shortened luteal phases which indicate deficiencies of progesterone. However, it is the follicular phase progesterone produced by the adrenal glands that moderate estrogen induced buildup of a thickened uterine lining.
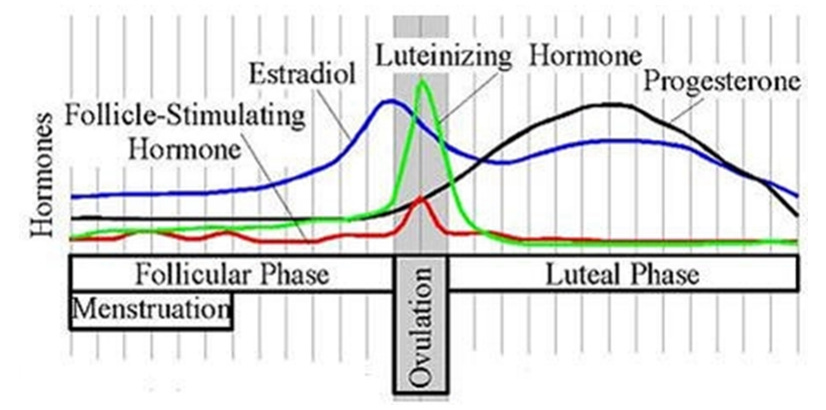
This is a commonly recognized depiction of the menstrual cycle. This graphic is a cause of the misconception about the importance of progesterone. It looks like it is insignificant in the follicular phase. However, the lines represent levels of hormones in two different units. The estrogens are measured in picograms/milliliter and progesterone is in nanograms/milliliter. This means that the black line for progesterone would be 1000 times higher if expressed in the same units the estrogen level is expressed. This graphic like many does not even indicate the units that generated this depiction. Using supplemental progesterone during the follicular phase can restore the proper balance in a cycle or two.
Not only that, but heavy bleeding has also been reversed with the use of vitamin A.
Vitamin A in the treatment of menorrhagia - PubMed (nih.gov)
Vitamin A is needed to produce progesterone from cholesterol.
4. Based on your experience, what percentage of women recommended for hysterectomy could be helped with hormone supplementation instead?
I think that nearly all could avoid surgery. Perhaps if there is a baseball sized fibroid, surgery might be indicated but why was progesterone not used when that fibroid had an insignificant size.
5. When you encounter women who have already had their uterus removed, how do you approach their post-surgery care? What treatments do you find most effective?
Sometimes, a women will have only the uterus removed and the ovaries are left intake. They are not offered any support. However, the stress of the surgery often causes diminished ovarian function and a multitude of hormone deficiencies as a consequence.
6. For women who have undergone oophorectomy (removal of ovaries), how does your treatment strategy change? How do you address the loss of natural hormone production?
There is no need to “test” for hormone deficiencies. The removal of an organ involved in significant production of hormones is not available. Now is the time to restore as many hormones as possible. These include progesterone, testosterone (50% gone), estrogens, and DHEA. Conventional medicine ignores all but estrogen. This continues the imbalance of hormones that lead to the hysterectomy in the first place.
7. From your perspective, why are gynecologists so quick to recommend surgery as the solution to issues that might be treated with hormone therapy?
It is an economic decision for the gynecologist. Gynecologists are surgeons. Restoring hormones is time consuming for practitioners and not as financially rewarding as a quick surgery.
8. Can you share a case where bioidentical hormone replacement therapy (BHRT) significantly improved the quality of life for a woman who had been advised to undergo a hysterectomy?
This should be the case 100% of the time. However, women don’t always get 100% relief even with bioidentical hormones when the practitioner does not partner with their patients to achieve that. Practitioners are trained in flow chart medicine and have great difficulty in helping women find their best dosing and combinations of hormones. I always encourage women to demand 100%. If they feel much better but not 100%, adjustments should be made.
9. What challenges do you face when advising against hysterectomy and advocating for hormone therapy? How do you overcome skepticism from patients or other healthcare providers?
The challenge is that women are frightened into surgeries and fast tracked before they have the time to think things through. Further, the consequences of surgery are minimized when presented. I don’t know how to help to get information to these women. Those that I can and do work with have self selected themselves by doing some research and are strongly against having surgery.
10. How does the absence of a uterus and/or ovaries affect a woman's hormone balance, and how do you address these changes with BHRT?
I think this was covered earlier but I would also like to bring up the distortion these surgeries create in the body. Organs take up space in the body and now shifts occurs because the placeholders are gone. Follow up surgeries may now be performed on the bladder because of the missing organs.
11. What misconceptions do you often encounter about hormone therapy among women advised to have a hysterectomy?
What exactly is hormone therapy? Is it the thousands of combinations of synthetic drugs or is it topping off hormones with those with the identical structure. Practitioners don’t think twice about prescribing antidepressants and antianxiety drugs with high risk effects and fight with their patients about restoring the most abundant sex hormone in the human body.
12. In your opinion, what are the long-term implications of hysterectomy and oophorectomy that women might not be fully aware of when they consent to surgery?
They are not told that their lives will be shorter, that they will suffer more from osteoporosis, that they may never have restorative sleep again, that they will suffer the loss of muscle mass from the lost testosterone, that they will be anxious, enraged, panicky and perhaps diagnosed with a mental illness, that they will be offered a long list of pharmaceuticals for symptom relief which will fail them, that their bodies will suffer with pain and the list goes on.
13. How do you monitor and adjust hormone therapy for women who have had their reproductive organs removed, ensuring they receive the most benefit?
You can test with many modalities, but the testing will verify absorption but not give you guidance with clinical relief. Women will tell you and you can see clinical signs.
14. Where can women go to get more information and support if they are considering alternatives to hysterectomy?
There are a few groups like Nora Coffey’s, HERS Foundation.
Social media has really helped. There are lots of Facebook groups of women trying to help each other that sometimes actually do help. Yes, you have to be careful. PhRMA has funded a lot of social media advocate groups which will try to minimize the consequences or advocate a surgery or drug solution.
15. Finally, can you share any resources, such as books, websites, or forums, where women can learn more about the benefits of hormone supplementation and the potential to avoid surgery?
No More Hysterectomies by Vicky Hufnagel
Estrogen Dominance Support Group on Facebook
If I do a Facebook search there is not very much about preventing hysterectomy, only coping. I found one Hysterectomy Hoax with only about 500 members.
Final Note
I’d like to reinforce the message that there are relief measures from the ravages of hysterectomy.
You can get your life back and even better.
There may be a progesterone conspiracy going on.
North American Menopause Society, American College of Obstetrics and Gynecology and the Endocrine Society have fostered this idea that women with hysterectomy do not need progesterone. It is heavily embedded into medical practice. If you check out Wikipedia on PMDD, premenstrual dysphoric disorder, which are simply the mood issues of PMS, premenstrual syndrome, progesterone is not mentioned. Indeed, the PMDDers are systematically taught all the way to the final solution of hysterectomy that they must avoid progesterone at all costs since they are somehow sensitive to it.
In the UK, family practitioners cannot prescribe more than 200 mg of progesterone. When the deficiency is severe, progesterone dosing must be very generous to get results.
And women are also being denied testosterone after oophorectomy. There are no FDA approved products for testosterone replacement in women in the US. Testosterone is far more abundant than estrogen in the human female body and is sorely needed by many surgical menopause or not.
Thank You for Being Part of Our Community
Your presence here is greatly valued. If you've found the content interesting and useful, please consider supporting it through a paid subscription. While all our resources are freely available, your subscription plays a vital role. It helps in covering some of the operational costs and supports the continuation of this independent research and journalism work. Please make full use of our Free Libraries.
Discover Our Free Libraries:
Unbekoming Interview Library: Dive into a world of thought-provoking interviews across a spectrum of fascinating topics.
Unbekoming Book Summary Library: Explore concise summaries of groundbreaking books, distilled for efficient understanding.
Hear From Our Subscribers: Check out the [Subscriber Testimonials] to see the impact of this Substack on our readers.
Share Your Story or Nominate Someone to Interview:
I'm always in search of compelling narratives and insightful individuals to feature. Whether it's personal experiences with the vaccination or other medical interventions, or if you know someone whose story and expertise could enlighten our community, I'd love to hear from you. If you have a story to share, insights to offer, or wish to suggest an interviewee who can add significant value to our discussions, please don't hesitate to get in touch at unbekoming@outlook.com. Your contributions and suggestions are invaluable in enriching our understanding and conversation.
Resources for the Community:
For those affected by COVID vaccine injury, consider the FLCCC Post-Vaccine Treatment as a resource.
Discover 'Baseline Human Health': Watch and share this insightful 21-minute video to understand and appreciate the foundations of health without vaccination.
Books as Tools: Consider recommending 'Official Stories' by Liam Scheff to someone seeking understanding. Start with a “safe” chapter such as Electricity and Shakespeare and they might find their way to vaccination.
Your support, whether through subscriptions, sharing stories, or spreading knowledge, is what keeps this community thriving. Thank you for being an integral part of this journey.





Number 12 fascinates me. (quoted below)
I know a number of elderly women who had hysterectomies earlier in life. These individuals are callous people at their best, and full-out sociopathic at their worst.
Society is experiencing a "loss of empathy" on an epic scale.
Makes me wonder if the loss of hormones (that contribute to nurturing, etc.) is part of that?!
***********************
"12. In your opinion, what are the long-term implications of hysterectomy and oophorectomy that women might not be fully aware of when they consent to surgery?
They are not told that their lives will be shorter, that they will suffer more from osteoporosis, that they may never have restorative sleep again, that they will suffer the loss of muscle mass from the lost testosterone, that they will be anxious, enraged, panicky and perhaps diagnosed with a mental illness, that they will be offered a long list of pharmaceuticals for symptom relief which will fail them, that their bodies will suffer with pain and the list goes on."
This sums it up:
In your opinion, what are the long-term implications of hysterectomy and oophorectomy that women might not be fully aware of when they consent to surgery?
They are not told that their lives will be shorter, that they will suffer more from osteoporosis, that they may never have restorative sleep again, that they will suffer the loss of muscle mass from the lost testosterone, that they will be anxious, enraged, panicky and perhaps diagnosed with a mental illness, that they will be offered a long list of pharmaceuticals for symptom relief which will fail them, that their bodies will suffer with pain and the list goes on.
I wrote a book about this subject, Hormone Secrets. The free download is here or you can buy a hard copy on Amazon. https://dl.bookfunnel.com/p7dvqow83g