Anaphrodisia
On Hysterectomy and Female Castration
In my early 20’s, a gynecologist told me that if I wanted to have a baby I’d better go ahead and do it and then everything would have to come out. My husband had been generously sharing his various diseases from his various liaisons and the treatments were taking their toll.
I didn’t know it but this was the same doctor who had tied my older sister’s tubes while she was under anesthesia (c-section) without her consent. He came out to the waiting room with bloody gloves and told her husband that it needed to be done and he was scared because of the blood and said okay. (I also didn’t know about the abortion clinic out back)
I dumped the doctor and the husband.
A few years later, I remarried after telling my husband-to-be that I probably couldn’t have a baby. He said it was okay but we’d try. We went on to have three babies. And the constant infections and other problems I thought were permanent went away with a clean sexual partner.
When I was a teenager (eons ago-late 60’s early 70’s) one of my mother’s friends confided that there had been a mistake in her daughter’s treatment. The young woman had stopped having periods and was hoping she was pregnant, so she went to the doctor. He told her it was a tumor-cancer-and removed her uterus. Inside the uterus, the pathologist found a fetus. - Candy Farnsworth
When I first awakened to childhood vaccination, I was in a daze at its magnitude and meaning. As we Australians would say, I was like a stunned mullet.
Well, I have a similar feeling now awakening to the subject of hysterectomies and female castration.
The sheer scale and mindless butchery of it all is something I’m struggling to comprehend.
This all started with my wonderful interview with Carol Petersen. If you missed it, I recommend reading it.
Hormones - Lies are Unbekoming (substack.com)
Towards the end of the interview, she said:
“Most reasons for hysterectomies can be tied to progesterone deficiencies and most could be avoided with rational supplementation.”
I did a double take on that sentence.
Are you telling me that women are having body parts removed, on scale, unnecessarily?
Yes, that is exactly what I was being told.
It led so far to these stacks:
Hysterectomy - Lies are Unbekoming (substack.com)
Female Castration - Lies are Unbekoming (substack.com)
And now to this one.
I think this should be mandatory reading for all women, because at some point a doctor or a gynecologist are very likely going to “suggest” a hysterectomy, and you need to be alert and armed with the necessary information to understand what is happening and how to keep the butcher at bay.
When I search Amazon with “hysterectomy” I get this:
Coloring books!!
I am not aware of a great current book warning women off hysterectomies and castration.
If you know of any, please let me know.
From what I can see the best books on the subject seem to have been written in the 1980s and they are just as relevant today as they were then.
One of the best books is The Castrated Woman by Naomi Miller Stokes.
Here is my book summary of it.
Seeing that it is a very hard book to get, and most people will not be able to access it. Here is the wonderful full Chapter 1, with some of my comments added.
Anyone thinking of giving up her uterus or ovaries should read this first.
The Castrated Woman by Naomi Miller Stokes.
Chapter 1 - HYSTERECTOMY: THE UNKINDEST CUT OF ALL
Hysterectomy is the most frequently performed major surgery in the United States.
It has become a growth industry, a very big business, with over $1.7 billion spent each year on the surgical procedure alone. The medical profession assures us that hysterectomy will continue to be an important part of the health care of American women in the years ahead. Which is very bad news, indeed.
The cost to women in terms of physiological and sexual dysfunction is staggering. Tragically, well over 90 percent of these operations are clearly unnecessary. Most of them could have been avoided by the use of alternative therapy. Many are done for downright foolish reasons. Of all the hysterectomies performed each year, about one out of five is for sterilization only, with absolutely no legitimate medical reason.
One of the most stunning aspects of this needless butchery is that the medical profession's marvelous new microsurgery techniques, the development of plastic surgery, ultra sound, and new knowledge about hormones actually make most of these surgeries unnecessary.
How prevalent is this blight? During the nine-year period from 1970 to 1978, approximately 3,536,000 young women between the ages of 14 and 44 had hysterectomies. In 1980, American physicians performed 649,000 reported hysterectomies. In 1981, the figure rose to 673,000 and dropped in 1982 to 650,000. In 1983 it soared to a whopping 672,000. Approximately one-half of all hysterectomies involve removal of the patient's ovaries.
I find this numbers staggering.
Relying on the 1980 Census data, the estimate of females between the ages of 14-44 in 1978 is 28.4m.
That means that 12% of females has their uterus removed. That is 1 in 8. I am struggling to wrap my head around these numbers.
That also means that 1 in 16, in this 14-44 cohort, had their ovaries removed. Were castrated!
These figures do not include women undergoing hysterectomy in federally operated hospitals, such as Armed Forces and Public Health Service hospitals, nor do they include the number of women who have undergone radical hysterectomy (removal of uterus, cervix, tubes, ovaries, adjacent lymph glands, and part of the vagina) or pelvic exenterations (even more radical removal of the lower bodily cavity such as all of the vagina and part of the bowel). Total number of hysterectomies done each year is conservatively estimated at over one million.
Women usually refer to the operation as being a "complete" hysterectomy, by which they mean the removal of the uterus, tubes, and ovaries. In medical terms, if both the Fallopian tubes and ovaries are removed, the operation is correctly called a total hysterectomy and bilateral (both sides) salpingo-oophorectomy (tubes and ovaries removed). It is a surgery that has been subjected to intense scrutiny in recent years by consumer groups, government agencies, insurance companies, and professional societies. Almost no one has spoken for the women who undergo the operation.
Hysterectomy is one of several surgical procedures which threaten human sexuality. Others are the "ostomies"-colostomy, cystostomy, and ileostomy. Colostomy is the formation of a surgical fistula, or opening, which periodically voids fecal matter from the large intestine into a bag. Cystostomy is a surgical opening from the bladder which voids into a bag. Ile ostomy is the formation of a surgical opening from the small intestine which drains continuously into a bag.
These are difficult surgeries. They have a dramatic effect on sexuality for both women and men. But hysterectomy rep resents a special peril all its own. One does not wear an ex ternal bag after the surgery. One need not fear the odor from escaping body fluids. The aftermath of hysterectomy for many women is much worse. They are left with anaphrodisia, or loss of sexual desire and feeling.
I wonder what the divorce rate is within this population of butchered women.
I wonder how many gynecologists, in seeking informed consent, tell the women, that the risk of divorce goes from X to Y?
The truth is that an appalling subculture of American women suffer in silence from a loss of sexual desire, or libido, as a result of this surgery. Whatever it is called, the result is the same. Women no longer have any desire to have sex with their husbands or lovers. The loss is not limited to heterosexual sex. Lesbian women report the same problem and are given the usual medical double talk and shuffled off for psychoanalysis.
"Don't worry about sex," said one doctor. "Hysterectomy isn't any worse than having your tonsils out."
Hysterectomy is much worse than having one's tonsils out. Research shows it is a surgery that wreaks far-reaching havoc, of which sexual dysfunction may be only one result.
A relatively new finding is that the hormonal changes brought about by hysterectomy frequently result in atherosclerotic heart disease. Four independent investigations have shown a three fold increase in such heart disease following hysterectomy. It is thought that prostacyclin, a potent vasodilator and inhibitor of platelet aggregation produced by the uterus, protects women who still have their uteruses from heart failure.
The book was published in 1986.
Here are more recent studies saying exactly the same thing.
A study highlighted by the American Heart Association News indicates that ovary-sparing hysterectomies might not protect women against metabolic syndrome, a cluster of conditions that elevate the risk of heart disease and stroke. The research showed that women who had undergone hysterectomy faced a 4.6-fold increased risk for heart failure and a 2.5-fold increased risk for heart disease, particularly among those aged 35 or younger.
Similarly, the Mayo Clinic reported that women undergoing hysterectomy with ovarian conservation, especially those at or before the age of 35, exhibited a significantly higher risk of developing cardiovascular conditions such as hyperlipidemia, hypertension, obesity, cardiac arrhythmias, and coronary artery disease. The study indicated a 4.6-fold increase in the risk of congestive heart failure and a 2.5-fold increase in the risk of coronary artery disease for this demographic.
Another serious side effect is post-hysterectomy syndrome, a nicer term for severe suicidal depression. Hysterectomy patients have double the number of postoperative admissions to psychiatric hospitals as do patients who have undergone other kinds of surgery. It is noteworthy that these patients have an important lack of prior psychiatric history.
The third side effect is the one talked about the least-the one thought for years to be nothing more than "old wives' tales" or sick fantasies indulged in by half-crazy menopausal women. This side effect has to do with the most intimate part of a woman's life-her sexuality.
Every woman faces the possibility that hysterectomy will be recommended at some time during her life. According to the figures, this will happen during her young womanhood. A detailed analysis performed by the National Center for Health Statistics (NCHS) reveals that in 1978, for example, 63 per cent of the women who underwent this operation were 15 to 44 years old, 31 percent were 45 to 64 years old, and only six percent were 65 or older.
In the United States the majority of hysterectomies are performed upon women during their reproductive years. Perhaps this is why approximately 27 percent of the women in this country of childbearing age can have no children. [This figure does not include women who are infertile.] According to a re port from the NCHS, of the 54 million women between the ages of 15 and 44, almost 9.5 million have chosen to be sterilized for reasons of birth control. An additional 4.2 million have been surgically sterilized for other reasons. And 4.4 million are so physically handicapped that conception and successful pregnancy would be either extremely difficult or downright impossible. According to the National Center, sterilization by surgery is the leading method of birth control in the United States. An appalling number of these sterilizations have been accomplished by hysterectomy.
Reading this passage, I cannot help but think about population control.
I’m reminded of NSSM 200 that I wrote about in Dec 2023.
NSSM 200 - Lies are Unbekoming (substack.com)
The overall strategy above provides a general approach through which the difficulties and dangers of population growth and related problems can be approached in a balanced and comprehensive basis. No single effort will do the job. Only a concerted and major effort in a number of carefully selected directions can provide the hope of success in reducing population growth and its unwanted dangers to world economic will-being and political stability. There are no "quick-fixes" in this field. Below are specific program recommendations which are designed to implement this strategy. Some will require few new resources; many call for major efforts and significant new resources. We cannot simply buy population growth moderation for nearly 4 billion people "on the cheap". - Page 84
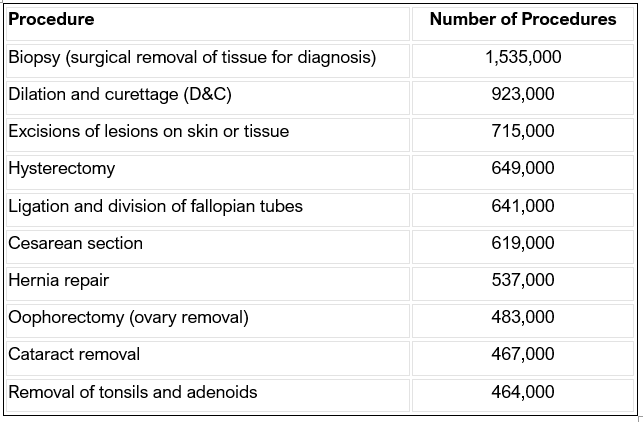
American women know the inside of operating rooms far too well. Of the ten most frequently performed surgical procedures, five are performed solely for women. According to the American College of Surgeons, the list of the ten most frequently performed surgeries (based on 1980 figures) are as follows:
Of all the adult women in the country today, 62 percent will have had a hysterectomy (removal of the uterus) and/or oophorectomy (removal of the ovaries) by the time they are sixty five or seventy.
The two surgeries are usually done simultaneously, with removal of the ovaries performed routinely as "part of the hysterectomy" when, in fact, the ovary removal is almost always entirely unnecessary. In many cases it is done as a prophylactic measure; the organs are removed "while the surgeon is in there anyway," before they become diseased.
Some women who have had hysterectomies do not know whether they have had their ovaries removed. Others agreed to the removal without really knowing what they were agreeing to, or without realizing that hysterectomy itself is an elective procedure. Few, if any, know anything at all about the dis advantages of such surgery.
That's the sort of thing that happened to Miranda J.
When I was twenty-two I got a pain in my abdomen. I went to the hospital. They told me they had to do an exploratory operation and shot me full of morphine. When I came to, my uterus and ovaries were gone.
I cried and screamed because I was so upset. I had wanted children. I asked them how they could do a thing like that to me. They said I had an infection, that be fore I went into surgery I had signed a paper saying anything they did was all right. I have no memory of signing anything.
Sex hasn't meant anything to me since that operation, although I really loved it before. The doctors told me to wait until I was in my late thirties when I would be at my prime. I'm thirty-seven now and still waiting. I haven't recovered my sex drive. When I ask them about it, they just shrug and say I'm very unusual.
The United States has twice the hysterectomy rate of England and Sweden. Doctors' wives have more hysterectomies proportionately than any other group. Black women have twice as many hysterectomies as white women, although poor white women are not exempt from hysterectomy being used as a form of sterilization abuse.
Countless welfare mothers have been given vaginal hysterectomies, which leave no abdominal scars, without their previous knowledge or consent. The medical profession terms this sort of surgery a Mississippi Appendectomy.
Hysterectomy rates, which vary substantially in different regions of the United States, are lowest in the west. The northeast is next in frequency, then the north central section of the country. The rate is highest in the south.
Total hysterectomies have been performed since the mid-1940s. Prior to that time, gynecologists and surgeons performed what were called "subtotal hysterectomies," a procedure which left a cervical stump. Subtotals were faster; the patient didn't have the opportunity to bleed as much as during a total hysterectomy. In those days there was usually a lack of adequate blood for transfusions.
In some cases the retained cervix became cancerous, although it is entirely possible that those women would have gotten cancer anyway. With the advent of improved surgical techniques and supporting technologies, total hysterectomy became the surgery of doctors' choice. Legal and social changes in the late 1960s, particularly the emphasis on limiting population (abortion was illegal), brought about increased acceptance of sterilization as a means of contraception. For the first time, gynecologists recommended that hospitals no longer require a medical staff committee to review requests for sterilization based on parity and age.
Dr. Ralph Wright, a Connecticut gynecologist and an out spoken advocate of hysterectomy, attempted to explain why tissue committees were being presented with such large numbers of manifestly healthy uteruses. Widely quoted in obstetrics and gynecology journals, he wrote and spoke of "radical changes" in indications for hysterectomy.
Concerning sterilization he wrote: "To sterilize a patient and allow her to keep a useless and potentially lethal organ is incompatible with modem gynecologic concepts. Hysterectomy is the only logical approach to surgical sterilization."
This was the same physician who wrote, regarding cancer prevention, "... when the patient has completed her family, total hysterectomy should be performed as a prophylactic procedure. Under these circumstances, the uterus becomes a useless, bleeding, symptom-producing, potentially cancer-bearing organ and, therefore, should be removed."
In response to Wright's mind-boggling pronouncement, Dr. Stanley Friedman replied: "From 1960 to 1965 the death rate from prostatic cancer was about equal to that from all uterine cancers (National Vital Statistics Division and Bureau of the Census, United States). Applying Wright's logic of 'one basic principle, ' it would seem equally rational to perform elective prostatectomy on every male whose wife is to undergo elective hysterectomy."
However, many physicians agreed with Dr. Wright's thinking, and still do. In his book, A Woman Talks with Her Doctor: A Comprehensive Guide to Women's Health Care, Dr. Charles E. Flowers, Jr., says: "Many women resist a hysterectomy because they associate the loss of their uterus with the loss of their femininity. I am fully aware that the loss of reproductivity can be threatening to many women, but the argument that the uterus is an essential aspect of femininity is simply not true. The uterus has one signal purpose: to carry and nourish the growing fetus. The uterus has no relationship whatsoever to a woman's sexuality or her ability to make love, sometimes the ovaries are removed because they are diseased or cancerous or the woman has endometriosis. Other times the ovaries are removed in conjunction with a hysterectomy as a preventive measure. However, if a woman is already menopausal, if she has already stopped menstruating, and she is having a hysterectomy for fibroids or some other condition, I believe her ovaries should be removed at the same time so they won't later become a source of ovarian cancer ...if the woman's sex life was good before the operation, it's going to continue to be good. Just because she can no longer ovulate or conceive does not mean she cannot enjoy sex and have a good strong orgasm."
Whether or not gynecologists agreed with either rationale, physicians attending a general meeting of the American College of Obstetricians and Gynecologists on June 15, 1971, voted by applause to support sterilization as an appropriate medical indication for hysterectomy.
Sterilization then became a primary indication for hysterectomy. Men whose religions forbade birth control or abortion welcomed it, as did their wives-at least until after the surgery was done.
Many men still think hysterectomy means open sesame for sex. Women report that after their surgeries they are approached in a sexual way by male business and social associates. The woman has been "cleaned out" so she's safe for sex. They don't have to worry about getting her pregnant.
A whopping 68.5 percent of the vaginal hysterectomies performed at the University Hospital and Wayne County General Hospital in Ann Arbor, Michigan, between 1965 and 1970 were sterilizations for "socioeconomic" and "multiparity" reasons.
In 1970, 20 to 25 percent of hysterectomies done at Los Angeles County University of Southern California Medical Center were solely or primarily for sterilization.
The rate of sterilization by hysterectomy rose 293 percent between June 1968 and January 1970. California Blue Cross reported an increase of 79 percent in hysterectomies during just the first six months of 1970. Of 242 selected hysterectomies performed at the time of cesarean sections at the University of Arkansas Medical Center between 1970 and 1974, 68 percent were for sterilization.
The total number of hysterectomies performed nationally, as reported by NCHS, rose from 525,000 in 1970 to 690,000 in 1973, an increase of more than 30 percent.
Were women developing a plague of pelvic disease across the country? No, only a plague of doctors. Shockingly, numerous findings prove that changes in hysterectomy rates vary in ways that correlate directly with the number of surgeons in a given area or the number of hospital beds available.
Retrospective reviews of hospital charts have repeatedly revealed that at least 30 percent of that bloody harvest was not medically justified; sterilization or so-called "cancer prevention" were the reasons.
In 1976 Blue Cross-Blue Shield advised subscribers to get a second and third opinion before agreeing to any elective surgery. The recommendation was based in part on various medical audits that showed that in many regions of the United States more than 40 percent of the hysterectomies and oophorectomies involved removal of normal organs.
In 1977 the hazards of indiscriminate surgery prompted a Congressional investigation. Predictably, the principal spokesman for the American Medical Association rose to the surgeons' defense. Dr. James H. Sammons, executive vice-president of the AMA, said the increase in hysterectomies was due to their elective use as a "convenient form of sterilization and to their prophylactic use to eliminate the possibility of uterine cancer in future years." Dr. Sammons asserted that while the surgery could not be considered clinically necessary for either of these reasons, it was "beneficial to women with excessive anxiety and therefore necessary."
How many surgeons would cure a man's anxiety about developing cancer of the penis by cutting it off? It's almost too ridiculous to mention, but that's exactly what's been happening to thousands of American women.
Cancer prevention is considered by some physicians to be an indication for hysterectomy itself; cutting an organ out before it has a chance to become cancerous. Complete hysterectomy to "prevent" cancer is being done every day in surgeries across the country. But certain physicians in positions of national leadership are distressed at the concept of hysterectomies being performed for preventive reasons.
Dr. Franz lngelfinger, distinguished gastroenterologist who edited the prestigious New England journal of Medicine from 1967 to 1977, declares: "Once a physician starts removing healthy tissue for fear of cancer, he's gone too far."
The most frequent reason women seek gynecological care is for periodic genital and breast examinations to detect cancer. PAP examinations can lead directly to hysterectomies by revealing an abnormal condition such as severe dysplasia (a form of endometriosis), carcinoma in situ (cancer of the uterus), or invasive carcinomas (cancers) of the cervix.
PAP examinations can also lead indirectly to hysterectomies. If, upon pelvic examination, the gynecologist finds an ab normal condition such as uterine myomas (tumor containing muscle tissue), mild cervical dysplasia (abnormal changes in cervix tissue), or minimal prolapse of the uterus without as sociated pain or pressure, he may recommend hysterectomy.
These conditions by themselves would not medically justify hysterectomy. The woman can easily be "sold" hysterectomy with the argument that the uterus will probably develop more disease in time so it would be a good idea to remove it before that happens.
Some surgeons recommend the procedure to alleviate what they call "the drudgery of the menses," and still others be cause it is beneficial to the physician himself. "It decreases the frequency of unpleasant, humiliating pelvic exams and allows better utilization of health personnel, facilities and time."
Removal of normal ovaries at the time of hysterectomy is a common procedure. It is felt by the medical profession that such removal saves the .01 percent of women who otherwise might die from ovarian cancer. (This is also assuming that hormonal replacement therapy does not increase the chance of developing a malignancy of any remaining organ such as the breasts or the liver.)
Removal of the ovaries is comparatively simple when done at the time of uterus removal. Some doctors say they might as well be removed when the uterus is taken out because they'll very likely be severely damaged by the surgical procedure it self.
Dr. David R. Reuben, in his book, How to Get More Out of Sex, claims: "Hysterectomy doesn't have to be the end of sex for a woman. Like the old hospital joke, hysterectomy only takes out the baby carriage-it leaves the playpen intact. Most hysterectomies, even if the ovaries are not actually removed, bring on a 'surgical menopause.' Since the ovaries are such delicate structures, the cutting and crushing that goes on generally puts them essentially out of business."
Women who have a history of cancer in their families may decide to have their ovaries removed at the time of hysterectomy as a preventive measure. But it must be pointed out that the metabolic and endoctrine disturbances that develop when oophorectomy is performed are not reversed by the customary estrogen replacement. Even a small increase in the frequency of atherosclerotic heart disease, which frequently results from the loss of ovarian and uterine function, could offset any potential gain from cancer prevention.
In discussing cancer prevention surgery, researchers assume that a woman freed of the risk of one type of cancer would not be subject to a disproportionately higher risk of death from another cause, such as heart failure. Also, hysterectomy is not always the preferred treatment of uterine cancers. It would seem that the benefits of prophylactic surgery have been greatly overestimated. There is less chance that a woman will die from uterine cancer than that she will die when a hysterectomy is performed.
What are the health risks of hysterectomy?
Death is, of course, always a concern when any major surgery is undertaken for purely elective reasons. Although the mortality rate is low, the number of hysterectomies performed each year is so large that the resultant number of deaths is substantial. Each year more than six hundred women die as a result of complications from hysterectomy. How many die later from what may be certainly called residual effects, no one knows. The reported mortality rate for abdominal hysterectomy is .17 percent and for vaginal hysterectomy, . 08 percent. These figures do not include women who died with pelvic malignancies.
Operative and postoperative complications are common with this type of surgery. These operative complications include bleeding as well as bladder, urethral, and rectal injuries suffered during surgery. If severe, such bleeding requires trans fusions. The other complications require corrective surgery either at the time of the operation or following surgery, if the damage is not discovered when it is done.
Winifred F., a forty-year-old mother of three, said that she suffered pain, discharge, and a general feeling of total exhaustion for weeks following her hysterectomy, which was done because she was having discomfort with her periods. Her doc tor told her it would be best to have "all that stuff taken out." She said she felt like she had an abscessed tooth at the top of her vaginal canal. When her fever shot to 104, she was rushed to the hospital, opened up again, and a large abscess was found. "I'm terribly angry at myself for allowing the surgery," Winifred says now. "I would have been much better off if I'd just walked out of that doctor's office."
Fever is the most common postoperative complication but hemorrhage and transfusion, urinary dysfunction, wound and pelvic infections, intestinal obstruction, and thromboembolic disease are far too frequent, according to researchers now studying the problem.
In a Stanford study, 7.5 percent of nonemergency abdominal hysterectomy patients experienced moderate to life threatening complications. The study showed there was some degree of morbidity in 64 percent of the nonemergency abdominal hysterectomy patients seven days after surgery.
In another study involving six hundred patients, 5 percent had a second operation-eight during the initial hospital stay, twenty-two returning to the hospital later. The second operations were for incisional hernias, intestinal obstruction, vaginal hemorrhage, intra-abdominal hemorrhage, septic vaginal or pelvic hematomas, stress incontinence, ovarian cysts, appendicitis, prolapsed Fallopian tubes, and ulcer in the sacral region.
There is little documentation on how rapidly hysterectomy patients recover their normal functional level. The sparse studies that exist indicate that hysterectomy patients report an aver age of 11.9 months to recover fully from surgery. This com pares with a three-month recovery period for cholecystectomy (gall bladder removal), appendectomy, or partial mastectomy patients.
Depression is a particularly common psychological disturbance following hysterectomy. A survey conducted in England showed that depression, both treated with antidepressive drugs and untreated, was suffered by 70 percent of the women who had undergone such surgery, compared to only 30 percent of women who had undergone different kinds of surgeries.
A significant increase in visits to physicians for "neuroses and psychiatric disorders" was reported in a study from Manitoba. Researchers say that most of this increase was ac counted for by women in the 20- to 39-year-old age group, particularly those who underwent removal of the ovaries.
One researcher in the United States found that 7 percent of 729 women who had undergone hysterectomy were referred to psychiatrists within a period of four and one-half years after their surgeries. This referral rate was two and one-half times the rate expected for a matched group of women in the general population. Of these psychiatric referrals, 80 percent occurred within the first two years following hysterectomy. Women undergoing hysterectomy in the absence of severe pelvic disease such as cancer were referred for psychiatric care twice as often as those who had severe pelvic disease.
A list of medically appropriate indications for hysterectomy was issued by the Professional Standards Review Organizations (PSRO) in 1977. Included were malignant and premalignant disease of the endometrium (mucus membrane of the uterus) and cervix; fibroma (tumor) of the cervix, fundus, or broad ligament; abnormal bleeding; and prolapsed uterus (protrusion of the uterus through the vaginal orifice). If the parts were close to malignant or infectious disease-such as cancer of the colon or tubal infections-or the conditions were in conjunction with vaginal repair, hysterectomy was also medically justified. Excluded from the list was sterilization in the absence of ongoing uterine disease.
Intended to include all acceptable medical indications for hysterectomy from saving life at one end to simply improving it at the other, these indications did not alone dictate hysterectomy as the only, or even the best, means of treatment.
The Executive Board of the American College of Obstetricians and Gynecologists distinguished five levels of urgency for hysterectomy: emergency, mandatory, urgent, advisable, and elective.
Examples of the five levels are: An emergency would be intra-abdominal hemorrhaging, such as that caused by a ruptured ectopic pregnancy. The presence of a malignancy like an adenocarcinoma of the endometrium would call for mandatory surgery. Abnormal uterine bleeding requiring further di agnostic evaluation or definitive treatment is urgent. The advisable level is characterized by a condition like pelvic relaxation, such as that associated with urinary stress incontinence. Elective surgical procedures are those such as sterilization for family planning purposes. Elective hysterectomies would also include those for prophylaxis against potential disease such as uterine cancer.
The PSRO medical indications for hysterectomy specifically state that sterilization by vaginal or abdominal hysterectomy is acceptable only in the presence of concomitant uterine disease. The Medicare law specifically excludes reimbursement of hysterectomy for sterilization.
Some physicians consider hysterectomy the treatment of choice for economically disadvantaged women because such women have a greater risk of malignancy and are less likely to seek medical care. They cannot afford it. Socioeconomically disadvantaged women are at the highest risk of developing cervical cancer. For reasons as yet unknown they are not as likely to develop endometrial cancer, however, as endometrial cancer primarily affects middle and upper income women.
To lessen the abuse of this crippling surgery for minor benefits to the patients and major economic benefits for the physician, some medical experts feel that the elective hysterectomy policy should be directed toward implementation of the standards of care as developed by the PSRO program and the reimbursement policy of the Department of Health and Human Services.
This is unlikely to become a reality, however. Small successes have been achieved in limiting the numbers of elective hysterectomies by medical audit and peer review in certain in dividual institutions. But attempting to audit hysterectomies on a continual basis at the national level would be a formidable task. Under the present conditions of reimbursement incentives, such an attempt could not succeed. To disapprove indications for hysterectomy such as sterilization would only encourage further misrepresentation of the diagnosis.
The written medical records are not reliable. In many cases the true indications for surgery are not included in a patient's hospital chart for reasons including peer review; non reimbursement; and patient, physician, or hospital religious affiliations that make it expedient to write in only approved reasons for hysterectomy such as "abnormal bleeding" and "prolapsed uterus." Although these two indications are consistent with a pathology report of "normal uterus," they would pass inspection faster than "back problem," which some surgeons give as indication for hysterectomy.
Indications for hysterectomies on hospital charts change to reflect the times. Now, more and more "prolapsed uteruses" are noted, the increase apparently due to changes in hospital practice to accommodate elective hysterectomy for sterilization if third-party payments for hysterectomies for sterilization are unpredictable.
Sometimes the decision for surgery is made primarily by the doctor, sometimes by the patient. Sometimes a woman thinks she herself has made the decision when, in fact, she has been subtly influenced by the doctor's sales pitch. Many women, after talking with their physicians, choose hysterectomy to avoid "messy" menstruation, to ensure a safe birth control method, or from a fear of future cancer.
Numerous findings indicate that changes in hysterectomy rates are not a function of changes in pelvic disease or age pat terns among women. Hysterectomy rates have been shown to correlate with the ratio of surgeon to patient and the availability of hospital beds. Also, when medical audits are enforced, the hysterectomy rates have dropped sharply.
A lot of hysterectomy involves salesmanship on the part of physicians. Unfortunately, it's all too easy for a woman to believe, consciously or subconsciously, that an organ she cannot see, that bleeds regularly, will eventually become cancerous especially if her doctor skillfully hints at this possibility.
Yet one patriarchal family doctor once said: "If women were not meant to have these parts after production of their families, nature would have arranged for them to dry up around age forty-five."
Thank You for Being Part of Our Community
Your presence here is greatly valued. If you've found the content interesting and useful, please consider supporting it through a paid subscription. While all our resources are freely available, your subscription plays a vital role. It helps in covering some of the operational costs and supports the continuation of this independent research and journalism work. Please make full use of our Free Libraries.
Discover Our Free Libraries:
Unbekoming Interview Library: Dive into a world of thought-provoking interviews across a spectrum of fascinating topics.
Unbekoming Book Summary Library: Explore concise summaries of groundbreaking books, distilled for efficient understanding.
Hear From Our Subscribers: Check out the [Subscriber Testimonials] to see the impact of this Substack on our readers.
Share Your Story or Nominate Someone to Interview:
I'm always in search of compelling narratives and insightful individuals to feature. Whether it's personal experiences with the vaccination or other medical interventions, or if you know someone whose story and expertise could enlighten our community, I'd love to hear from you. If you have a story to share, insights to offer, or wish to suggest an interviewee who can add significant value to our discussions, please don't hesitate to get in touch at unbekoming@outlook.com. Your contributions and suggestions are invaluable in enriching our understanding and conversation.
Resources for the Community:
For those affected by COVID vaccine injury, consider the FLCCC Post-Vaccine Treatment as a resource.
Discover 'Baseline Human Health': Watch and share this insightful 21-minute video to understand and appreciate the foundations of health without vaccination.
Books as Tools: Consider recommending 'Official Stories' by Liam Scheff to someone seeking understanding. Start with a “safe” chapter such as Electricity and Shakespeare and they might find their way to vaccination.
Your support, whether through subscriptions, sharing stories, or spreading knowledge, is what keeps this community thriving. Thank you for being an integral part of this journey.


Same in the UK. I needed an investigation for a lesion and was told they would do a hysterectomy while they were in there. The justifications being that if they had to open me up to look they might as well remove it all as I was done with needing it any more, being over childbearing age.
That I said no was a total surprise to them, but despite more pressure from them I held my ground. I was traumatised by the experience for a long time, I know I would have ended up with even more trauma had I gone along with it just because the 'specialist' white coat told me to, with no medical justification.
Candy Farnsworth quote is astounding... I had no idea about this hidden sterilization agenda... and the compliance of doctors is staggering (whether they know what they're doing or not... These days it seems the doctors know very little about biology and seemed to be more trained in following procedure or handing out medication).
I know someone who had a hysterectomy in the 70's and it has played merry hell with her life since, I'm short on exact details, but a bladder displacement and all sorts of consequences for the organs in that region since that time, very painful.