Vaccination and Neurodevelopmental Disorders (Brain Inflammation and Damage)
A Study of Nine-Year-Old Children Enrolled in Medicaid – 25 Q&As
“I wonder if an 'epidemic' of regressive or sudden onset deafness were just treated as 'of concern?' or actually a crisis or emergency.”
It truly defies comprehension how people have been trained to callously dismiss, deny, and be unconcerned about child after child being unable to speak (!), despite working vocal cords, being unable to imitate (!), and thus learn, and being unable to interact normally and socially with others (!), all of which lead to isolation, dependence on others, and an inability to participate in society. What an astounding feat to get the majority of people to be unconcerned about such widespread devastation among our children, and further, to get them to be blind, deaf, and dumb to the main culprit (vaccines).
- Laura
For those of us that know about The Poisoning, this recent study just confirms what we already know.
For the rest, this important study hopefully creates a crack in the matrix.
The scale of the study is significant and the data we now have about vaccinating preterm births is also important.
There are aspects of the language in the study that I don’t like such as this at the end:
These results signal an urgent need for research to identify biological mechanisms and potential causal relationships between individual vaccines, or combinations of vaccines, and genetic, epigenetic, environmental and other biologic risk factors associated with NDDs.
We already know what the biological mechanisms are, it doesn’t need more research, just ask Dr Christopher Exley and Guillemette Crépeaux.
Toxins inflame babies’ brains. It’s that simple. Vaccines create childhood encephalitis. No more research is required.
This insistence on the sprinkling of genetic and epigenetic distractions into the mix is just that, a distraction. As I wrote a long time ago, and I repeat:
Autophagy - Lies are Unbekoming
Hmmm. Let’s see if I understand this. There are 100+ genes, that by themselves, or in combination, when interacting with their “environment” can “increase the risk” of ASD.
I think that’s like saying that a blind, deaf and mute man (having three genetic markers) was quietly walking down a sidewalk, when he fell into a gaping hole in the sidewalk (environmental factor), and ultimately to his death. I can see geneticists writing volumes of books on how his genetic markers led to his demise, while ignoring, silencing, cancelling, defunding, anyone who wanted to talk about the hole in the sidewalk. That’s modern-day genetics.
If it wasn’t for the aluminum in the body (the hole in the sidewalk), none of the genetic markers would matter.
With that out of the way, I’m glad we have the study.
With thanks to Anthony R. Mawson and Binu Jacob.
Related Posts
Deep Dive Conversation Library (Bonus for Paid Subscribers Only)
This deep dive is based on the study’s contents.
Discussion No.27:
20 important insights from this recent study: “Vaccination and Neurodevelopmental Disorders”
Thank you for your support.
Analogy
Imagine a garden where each plant represents a child's developing nervous system. Like all gardens, some plants naturally grow in more challenging conditions (preterm births) while others start with more favorable conditions (full-term births). Now, think of vaccinations as a type of fertilizer treatment - something introduced to protect and strengthen the plants.
In this garden study, researchers observed two large sections: one where plants received multiple fertilizer treatments (vaccinated children) and another where plants grew without these treatments (unvaccinated children). What they discovered was fascinating - while the fertilizer was intended to protect the plants, some plants showed unexpected changes in their growth patterns after receiving it. More notably, the plants that received multiple treatments (more vaccination visits) showed more significant changes in their development.
The most striking observation came from the section with naturally vulnerable plants (preterm births). When these delicate plants received the same fertilizer treatment as their hardier counterparts, they showed much more dramatic changes in their growth patterns. However, the vulnerable plants that didn't receive the treatment grew surprisingly similarly to their hardier untreated neighbors, suggesting that their initial vulnerability wasn't the primary factor in their altered development - it was the interaction between their vulnerability and the treatments.
12-point summary
Unprecedented Scale and Scope: This groundbreaking study examined 47,155 children in Florida's Medicaid program, representing one of the largest comparative analyses of vaccinated versus unvaccinated children ever conducted. The nine-year follow-up period provided exceptional depth in tracking developmental outcomes.
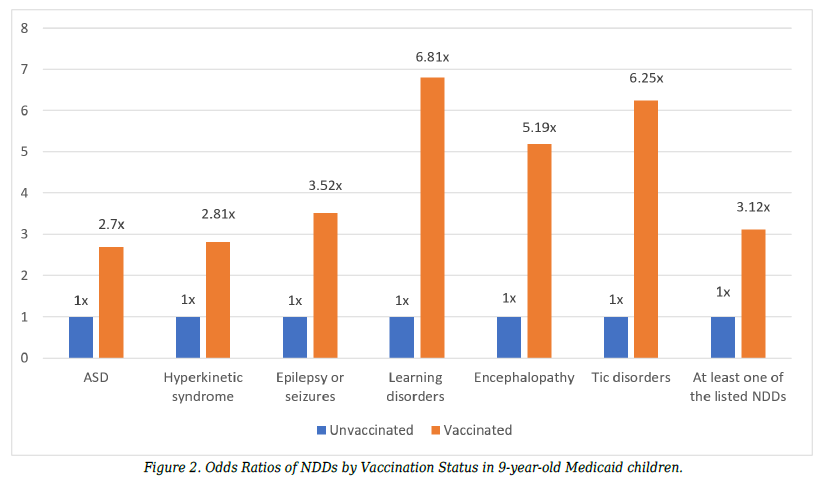
Clear Statistical Correlation: The research revealed that vaccinated children were 3.12 times more likely to develop a neurodevelopmental disorder compared to unvaccinated children. This finding was consistent across multiple types of disorders and demonstrated strong statistical significance with p-values less than 0.0001.
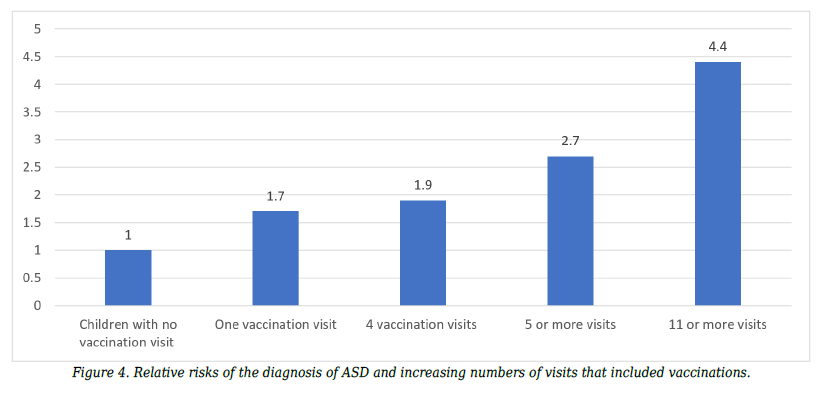
Dose-Response Relationship: Perhaps the most compelling finding was the clear dose-response relationship between vaccination visits and autism spectrum disorder. Children with eleven or more vaccination visits were 4.4 times more likely to develop ASD compared to unvaccinated children, suggesting a cumulative effect.
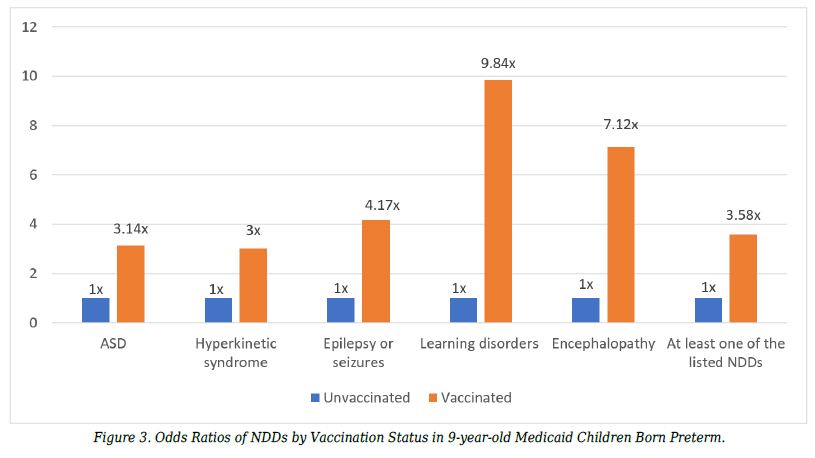
Preterm Birth Vulnerability: The study uncovered a crucial finding regarding preterm infants - when vaccinated, they showed dramatically higher rates of NDDs (39.9%) compared to unvaccinated preterm infants (15.7%). This suggests that preterm infants may be particularly susceptible to adverse effects from vaccination.
Demographic Patterns: The research revealed significant racial and ethnic disparities in vaccination rates, with European Americans showing the highest vaccination rate (94.2%) and African Americans the lowest (84.2%). These patterns persisted across both full-term and preterm births.
Multiple NDDs Affected: The study found increased risks across all examined neurodevelopmental disorders in vaccinated children, with odds ratios ranging from 2.7 for ASD to 6.8 for learning disorders. This comprehensive pattern suggests a broader impact on neurological development.
Temporal Relationships: The research established clear temporal sequences between vaccination and diagnoses, with the average first vaccination occurring at one year and two weeks, and average ASD diagnosis at six years and five months, supporting the possibility of causative relationships.
Preterm Protection: A remarkable finding showed that unvaccinated preterm infants had similar NDD rates to unvaccinated full-term infants (except for epilepsy/seizures), suggesting that prematurity alone may not significantly increase NDD risk without vaccination exposure.
Statistical Rigor: The study employed multiple statistical methods, including odds ratios, confidence intervals, and z-scores, with results showing extremely high statistical significance. Z-scores ranging from 4.4 to 24.7 standard deviations indicated highly unusual distribution patterns.
Methodological Strengths: The research design included comprehensive vaccination tracking through 326 different medical codes, continuous enrollment monitoring, and multiple analytical approaches, providing robust data validation.
Healthcare Implications: The findings challenge current vaccination practices, particularly the one-size-fits-all approach to preterm infant vaccination. The research suggests a need for more individualized vaccination protocols based on patient risk factors.
Future Directions: The study calls for urgent research into biological mechanisms linking vaccination and NDDs, emphasizing the need to understand cumulative effects rather than just individual vaccine safety, and recommending a pause in schedule expansion until more comprehensive research is completed.
Steve Kirsch
Summary
This is the best study to date confirming that vaccines are causing most of the autism in America due to the dose response relationship of the number of vaccine office visits and autism. I was EASILY able to replicate the odds ratios in a reader survey of 10,000 parents. It took about 24 hours to gather the data. My data was exclusively based on the total # of vaccines a child received, and not at all on the number of office visits. My odds ratio (OR) was 4.5. Mawson found RR=4.4 (the RR is generally slightly lower than the OR so these numbers are very similar).
It is telling that Congress will not require the NIH to do a study comparing the unvaccinated and vaccinated and that the NIH won’t do it on their own. NOBODY is calling for such a study (for some reason).
Sadly, it will likely take 50 years before such a study is done. In the meantime, don’t expect a single prominent mainstream doctor or academic to ever read this paper (or ask to see the data) until then.
25 Questions & Answers
Question 1: What was the primary objective of this research study and what population did it examine?
The research aimed to determine the association between vaccination and neurodevelopmental disorders (NDDs) in 9-year-old children enrolled in Florida's Medicaid program. The study examined 47,155 children who were enrolled in Medicaid from birth through age nine during the years 1999-2011. Three specific hypotheses were tested: whether vaccination was associated with autism spectrum disorder and other NDDs, whether preterm birth coupled with vaccination increased NDD odds compared to preterm birth without vaccination, and whether increasing numbers of vaccinations correlated with increased autism risks.
The study population included both full-term and preterm births, with 42,032 children (89.1%) receiving at least one vaccination and 5,123 children (10.9%) having no record of vaccination. This population represented Florida's fourth-largest Medicaid enrollment in the nation, comprising approximately 63% of birth deliveries and 47% of children in the state, making it a significant sample for analysis.
Question 2: How did the researchers identify and classify vaccinated versus unvaccinated children in the study?
Vaccinated children were identified through healthcare visits that included any vaccination-related codes in their Medicaid claims records. The researchers utilized a comprehensive list of 326 vaccine-related CPT, ICD-9, and NDC codes to identify vaccination status. These codes included all possible vaccination procedures, from routine childhood immunizations to adult vaccines and those for tropical diseases, ensuring thorough classification.
Unvaccinated children were defined as those without any claims records containing vaccination-related codes. The researchers acknowledged potential classification challenges, particularly regarding vaccinations administered outside the Medicaid system through programs like the Florida Vaccines for Children Program. They addressed this by using continuous enrollment data and comprehensive code lists to minimize misclassification, resulting in 10.9% of the study population being classified as unvaccinated.
Question 3: What specific neurodevelopmental disorders (NDDs) were examined in this research?
The study investigated six primary categories of neurodevelopmental disorders, each identified through specific diagnostic codes in the medical records. The conditions examined included autism spectrum disorder (ASD), hyperkinetic syndrome of childhood, epilepsy or seizures, learning disorders (identified through speech and language services), encephalopathy, and tic disorders. Each disorder was tracked using specific ICD-9-CM diagnostic codes, allowing for precise identification and classification.
These disorders were selected based on their prevalence in childhood development and their potential relationship to environmental factors. The research particularly focused on the relationship between these disorders and vaccination status, examining both individual conditions and the presence of at least one NDD in study participants, providing a comprehensive view of neurodevelopmental outcomes.
Question 4: What was the significance of choosing the 9-year age group and Florida Medicaid population for this study?
The selection of 9-year-olds aligned with the CDC's approach to monitoring autism prevalence, which typically uses 8-year-olds as a benchmark. This age selection provided sufficient time for diagnosis of various NDDs while ensuring complete vaccination histories could be analyzed. The Florida Medicaid population offered a large, diverse sample with continuous enrollment data, allowing researchers to track health outcomes from birth through childhood.
The Medicaid population also provided unique advantages for the study, as it included a higher proportion of at-risk children based on the Healthy Start Infant Screening Tool. This population typically requires greater screening for developmental problems, making it particularly relevant for studying neurodevelopmental outcomes. Additionally, Florida's position as the fourth-largest Medicaid population in the nation provided a substantial sample size of 47,155 children.
Question 5: How did the researchers control for potential confounding factors in their analysis?
The researchers implemented several control measures to address potential confounding factors. They adjusted for age by limiting the study group to children from birth to age 9 (108 months) and ensured comparable gender distribution between vaccinated and unvaccinated groups, with both showing a higher proportion of males (53%) than females (47%). The large study population of 47,155 children helped minimize the impact of individual variations.
While technical limitations prevented the exclusion of children with congenital anomalies, the researchers demonstrated that this likely had minimal impact due to the very small percentage (0.5%) of affected children in the population. They supported this assertion with comparative data from Denmark showing similar low percentages (0.1%) of children affected by these conditions, suggesting these factors would not significantly influence the study's findings.
Question 6: What role did the DEVEXI platform play in data collection and analysis?
The DEVEXI platform served as an integrated health and medical research platform for generating epidemiological studies. It provided access to comprehensive Florida Medicaid claims data, including procedure records, medications, diagnosis codes, demographics, medical and dental claims, and costs for all procedures, treatments, and drugs. The platform ensured HIPAA compliance and met U.S. government guidelines for data de-identification, data safety, and security.
DEVEXI utilized Amazon Redshift for complex analytic queries in the cloud and incorporated rigorous data de-identification processes following the 2012 Office for Civil Rights guidelines. This included removing 18 types of patient identifiers while maintaining the ability to track individuals through unique alphanumeric codes, enabling accurate longitudinal analysis without compromising privacy. The researchers were among the first to test and operate the initial version of DEVEXI, receiving technical assistance throughout their research.
Question 7: How were vaccination visits quantified and measured throughout the study?
Vaccination status was determined by tracking healthcare visits that included vaccination-related billing codes in the Medicaid claims records. A visit with vaccination was defined as a billing claim containing at least one vaccine-related code recorded in a patient's medical record on a given day. The researchers noted that by age two years, 17% of children had no vaccination record, and only 44% had four or more visits with vaccinations.
For the third aim of the study examining dose-response relationships, the researchers analyzed children from birth to age five years who received at least one or more visits with vaccinations (n=41,033), and then tracked ASD diagnoses from ages five to nine. This approach allowed them to establish temporal relationships between vaccination exposure and subsequent diagnoses while accounting for the typical age of ASD diagnosis in the Medicaid population.
Question 8: What specific medical coding systems were used to track diagnoses and vaccinations?
The study utilized three primary coding systems to track both vaccinations and diagnoses: Current Procedural Terminology (CPT) codes, International Classification of Diseases (ICD-9) codes, and National Drug Codes (NDC). For vaccination identification alone, the researchers employed 117 CPT codes, 18 ICD-9 codes, and 191 NDC codes, creating a comprehensive system for identifying any vaccination-related healthcare encounter.
These coding systems were also used to identify specific conditions and diagnoses. For example, live births were tracked using V30-V39 series ICD-9 codes, preterm births were identified using code 765 series, and each NDD had its own specific set of diagnostic codes. This multi-coding approach helped ensure accurate identification of both exposures (vaccinations) and outcomes (NDDs) throughout the study period.
Question 9: How did researchers ensure data accuracy and privacy compliance?
The research team implemented multiple layers of privacy protection and data accuracy measures. The DEVEXI platform complied with HIPAA requirements and was certified by Westat as meeting U.S. government guidelines for data de-identification, safety, and security. Individual identifiers were replaced with unique alphanumeric codes that allowed tracking across multiple visits and providers while maintaining anonymity.
To ensure accuracy, the researchers used comprehensive lists of medical codes and validated their findings against preliminary assessments conducted by the Florida Department of Health query system. They also employed multiple verification steps, including checking for duplicate records and implementing proper event sequencing functionality. The research was conducted in accordance with all relevant guidelines and regulations, without requiring institutional review board approval due to the de-identified nature of the data.
Question 10: What statistical methods were employed to analyze the relationships between vaccination and NDDs?
The researchers employed different statistical methods for their cross-sectional and retrospective cohort analyses. For the first two aims, they calculated prevalence odds ratios with 95% confidence intervals to test associations between vaccination and NDDs. Z-scores were computed to describe how far values deviated from the mean, with scores above 3.0 considered highly unusual.
For the third aim examining ASD specifically, they used Yates-corrected chi-square tests to calculate relative risks, providing more conservative estimates. They analyzed five different levels of comparison, ranging from one vaccination visit versus no vaccination to eleven or more visits versus no vaccination. This approach allowed them to examine potential dose-response relationships while maintaining statistical rigor through appropriate corrections and confidence intervals.
Question 11: What were the overall vaccination rates found in the study population?
Among the total study population of 47,155 children, 42,032 (89.1%) had received at least one vaccination by age nine. The vaccination rates remained notably consistent across birth years from 1999 to 2002, with minimal variation ranging from 88.7% to 90.0%. This stability in vaccination rates demonstrated consistent healthcare practices throughout the study period.
When examining specific subgroups, vaccination rates showed variations by racial and ethnic categories. European American children had the highest vaccination rate at 94.2%, followed by Hispanic children at 92.5%. African American children showed a lower vaccination rate at 84.2%, representing the highest proportion of unvaccinated children at 15.8% of their demographic group. These patterns remained similar when analyzing both full-term and preterm births.
Question 12: How did NDD rates differ between vaccinated and unvaccinated children?
The research revealed substantial differences in NDD rates between vaccinated and unvaccinated groups. Overall, 27.8% of vaccinated children had been diagnosed with at least one NDD, compared to 11% of unvaccinated children. This translated to vaccinated children being 3.12 times more likely to be diagnosed with an NDD (95% CI: 2.85, 3.41).
Looking at specific disorders, vaccinated children showed significantly higher rates across all measured NDDs. The odds ratios ranged from 2.7 for ASD to 6.8 for learning disorders. The statistical significance of these differences was highlighted by z-scores ranging from 4.4 to 24.7 standard deviations from the mean, indicating highly unusual distribution patterns that strongly suggested non-random associations.
Question 13: What gender and racial/ethnic patterns emerged in the data?
The study population showed a consistent gender disparity, with males comprising 52.9% and females 47.1% of the total sample. This pattern held true across both vaccinated and unvaccinated groups, with slightly higher proportions of males in both categories. African Americans represented the largest racial group at 39.2% of the study population, followed by European Americans at 22%, and Hispanics at 19.8%.
Vaccination rates varied significantly by racial/ethnic group, revealing important disparities in healthcare utilization. European Americans showed the highest vaccination rate at 94.2%, while African Americans had the lowest at 84.2%. This pattern persisted even when controlling for preterm birth status, suggesting that racial disparities in vaccination rates were independent of other health factors.
Question 14: What were the most significant odds ratios discovered for various NDDs?
The study found striking odds ratios across all examined neurodevelopmental disorders. Learning disorders showed the highest disparity, with vaccinated children being 6.81 times more likely to receive this diagnosis compared to unvaccinated children. Tic disorders followed with an odds ratio of 6.25, and encephalopathy showed an odds ratio of 5.19.
Other significant findings included epilepsy or seizures with an odds ratio of 3.52, and hyperkinetic syndrome with an odds ratio of 2.81. Autism Spectrum Disorder showed an odds ratio of 2.70. All these associations demonstrated strong statistical significance with p-values less than 0.0001, indicating these relationships were highly unlikely to have occurred by chance.
Question 15: How did the timing of vaccinations relate to NDD diagnoses?
The researchers established specific time intervals to examine the relationship between vaccination timing and NDD diagnoses. For autism spectrum disorder specifically, they analyzed vaccination exposure from birth to age five years and subsequent diagnoses between ages five and nine. This approach ensured that vaccination exposure preceded diagnosis, strengthening the temporal relationship between the variables.
The average age of first vaccination visit was one year and two weeks, while the average age of ASD diagnosis was six years and 5.3 months. For children with 11 or more vaccination visits, the average age of vaccination visits was 3 years and 9 months, with an average ASD diagnosis age of 6 years and 4.3 months, demonstrating a consistent temporal pattern between exposure and diagnosis.
Question 16: How did preterm birth status affect the relationship between vaccination and NDDs?
Among the 5,009 preterm children in the study, vaccination status dramatically influenced NDD outcomes. Preterm children who were vaccinated (89.7%) showed significantly higher rates of NDDs compared to unvaccinated preterm children (10.3%). The most striking finding was that 39.9% of vaccinated preterm children were diagnosed with at least one NDD, compared to only 15.7% of unvaccinated preterm children, resulting in an odds ratio of 3.58.
The combination of preterm birth and vaccination appeared to create a synergistic effect. When examining specific NDDs, preterm vaccinated children showed significantly higher odds for all conditions except tic disorders. For instance, they were 3.14 times more likely to develop ASD, 9.84 times more likely to have learning disorders, and 7.12 times more likely to develop encephalopathy compared to unvaccinated preterm children.
Question 17: What were the specific findings regarding preterm infants who remained unvaccinated?
A remarkable finding emerged when comparing unvaccinated preterm infants to unvaccinated full-term infants. Aside from epilepsy or seizures, which showed a significant difference (4.8% vs. 2.2%), unvaccinated preterm children demonstrated remarkably similar NDD rates to their full-term counterparts. This suggests that preterm birth alone, without vaccination, did not substantially increase the risk of most NDDs.
The evidence showed minimal differences in other NDDs between unvaccinated preterm and full-term children: ASD (1.5% vs. 1%), hyperkinetic syndrome (10% vs. 8.4%), learning disorders (0.6% vs. 0.4%), and encephalopathy (1% vs. 0.5%). These differences were not statistically significant, indicating that prematurity itself may not be the primary risk factor for NDDs when vaccination is not involved.
Question 18: What was the dose-response relationship between vaccination visits and ASD diagnosis?
The research revealed a clear dose-response relationship between the number of vaccination visits and ASD diagnosis. Children with just one vaccination visit were 1.7 times more likely to be diagnosed with ASD than unvaccinated children. This risk increased progressively with additional vaccination visits, demonstrating a consistent pattern of elevated risk with increased exposure.
The relationship became more pronounced with higher numbers of vaccination visits. Children with 1-4 vaccination visits were 1.9 times more likely to receive an ASD diagnosis than unvaccinated children, while those with 5 or more visits showed 2.7 times higher risk. The highest risk was observed in children with 11 or more vaccination visits, who were 4.4 times more likely to be diagnosed with ASD compared to unvaccinated children, suggesting a strong dose-dependent relationship.
Question 19: How did ASD rates differ between children with varying numbers of vaccination visits?
The data showed a progressive increase in ASD rates correlating with the number of vaccination visits. Among children with no vaccination visits, the ASD rate was 0.9%. This increased to 1.5% for children with one vaccination visit, and further rose to 1.7% for those with one to four visits. The rate continued to climb, reaching 2.4% for children with five or more vaccination visits.
The most striking difference appeared in children with 11 or more vaccination visits, where the ASD rate reached 4.0%. This represented a 4.4-fold increase compared to unvaccinated children (95% CI: 2.85, 6.84). These findings maintained statistical significance even after controlling for various demographic factors, suggesting a robust association between vaccination frequency and ASD risk.
Question 20: What were the primary strengths of this research design?
The study demonstrated several methodological strengths, particularly in its representativeness and data quality. The large sample size of 47,155 children provided robust statistical power, while the continuous enrollment requirement ensured complete health histories. The study population's NDD and preterm birth rates aligned well with state and national statistics, suggesting strong external validity.
Another key strength was the comprehensive approach to identifying vaccinations and diagnoses through multiple coding systems. The research team used 326 different vaccination-related codes, including CPT, ICD-9, and NDC codes, to ensure accurate classification of vaccination status. Additionally, the nine-year follow-up period allowed sufficient time for NDDs to be diagnosed and documented, providing a complete picture of developmental outcomes.
Question 21: What limitations did the researchers identify in their methodology?
The researchers acknowledged several significant methodological constraints, with the Medicaid billing claims database presenting unique challenges. As claims data differs from medical records, coding errors could potentially result in misclassification of diagnoses. A specific example highlighted was the Hepatitis B vaccination timing, where although recommended at birth, the first recorded vaccination visit might appear several days later in the claims data, creating temporal accuracy issues.
The validation of vaccine uptake posed another substantial challenge due to the voluntary nature of Florida's centralized immunization registry reporting. The researchers faced difficulties in verifying vaccination status for children who may have received vaccines through external programs like the Florida Vaccines for Children Program or at facilities not captured in Medicaid claims data, such as schools, free clinics, or pharmacies. This limitation potentially affected the accuracy of the unvaccinated group classification.
Question 22: How might these limitations affect the interpretation of the results?
The potential misclassification of vaccination status could have influenced the study's findings in several ways. If vaccinated children were incorrectly classified as unvaccinated due to receiving vaccines outside the Medicaid system, this would likely result in an underestimation of the true differences between vaccinated and unvaccinated groups. The relatively high rate of unvaccinated children in the sample (10.9%) compared to national averages suggests some degree of misclassification may have occurred.
The reliance on claims data rather than comprehensive medical records might have affected the timing and accuracy of NDD diagnoses. However, the researchers argue that the large sample size and consistent patterns across multiple years and conditions help mitigate these concerns. Additionally, the dose-response relationship observed between vaccination visits and NDDs suggests that even if some misclassification occurred, the fundamental associations remained robust.
Question 23: What policy implications did the researchers draw from their findings?
Based on their findings, the researchers suggested that the current vaccination schedule may be contributing to multiple forms of neurodevelopmental disorders. They emphasized that while previous studies have focused on individual vaccines' safety, the cumulative impact of the expanded vaccination schedule on children's overall health has remained largely unexplored. This gap in understanding led them to advocate for a more comprehensive evaluation of the current vaccination schedule's impact on child development.
The researchers particularly highlighted the implications for preterm infants, who showed significantly higher risks when vaccinated. They questioned the current practice of vaccinating preterm newborns on the same schedule as full-term infants, suggesting that this one-size-fits-all approach might need reconsideration. The synergistic effect observed between preterm birth and vaccination indicated a need for more individualized vaccination protocols based on birth status.
Question 24: What recommendations were made regarding future vaccination schedules?
The researchers advocated for a pause in adding new vaccines to the federally recommended childhood vaccination schedule until more comprehensive research could be completed. They emphasized that new vaccines continue to be added under the assumption that they will have no effect on health beyond protection against targeted pathogens. However, their findings suggested that this assumption might need reevaluation, particularly regarding the cumulative effects of multiple vaccinations.
The study results led to recommendations for a more cautious and evidence-based approach to vaccination scheduling, particularly for vulnerable populations like preterm infants. The researchers suggested that the current practice of administering the same vaccination schedule to all infants, regardless of their birth status, should be reconsidered in light of the significantly increased risks observed in preterm vaccinated children compared to their unvaccinated counterparts.
Question 25: What further research did the authors suggest was needed?
The researchers called for urgent investigation into the biological mechanisms and potential causal relationships between vaccines and neurodevelopmental outcomes. They emphasized the need to understand how individual vaccines, or combinations of vaccines, might interact with genetic, epigenetic, and environmental factors to influence neurodevelopmental disorders. This research would help identify specific risk factors and potentially vulnerable populations.
They also highlighted the importance of studying the cumulative effects of multiple vaccinations, rather than just individual vaccine safety. The dose-response relationship observed with ASD suggested that the total vaccination burden might be more relevant than any single vaccine. The researchers advocated for comprehensive studies examining the overall impact of the vaccination schedule on children's health before any additional vaccines are added to the recommended schedule.
I appreciate you being here.
If you've found the content interesting, useful and maybe even helpful, please consider supporting it through a small paid subscription. While everything here is free, your paid subscription is important as it helps in covering some of the operational costs and supports the continuation of this independent research and journalism work. It also helps keep it free for those that cannot afford to pay.
Please make full use of the Free Libraries.
Unbekoming Interview Library: Great interviews across a spectrum of important topics.
Unbekoming Book Summary Library: Concise summaries of important books.
Stories
I'm always in search of good stories, people with valuable expertise and helpful books. Please don't hesitate to get in touch at unbekoming@outlook.com
For COVID vaccine injury
Consider the FLCCC Post-Vaccine Treatment as a resource.
Baseline Human Health
Watch and share this profound 21-minute video to understand and appreciate what health looks like without vaccination.










Vaccinations are a spiritual, satanic child sacrifice. Hence, the religious exemption.
The jabs give to the little children OCD of varying severity - so easier to brainwash.