The Rise and Fall of the Prostate Cancer Scam
By Dr Anthony Horan – 40 Questions & Answers – Unbekoming Book Summary
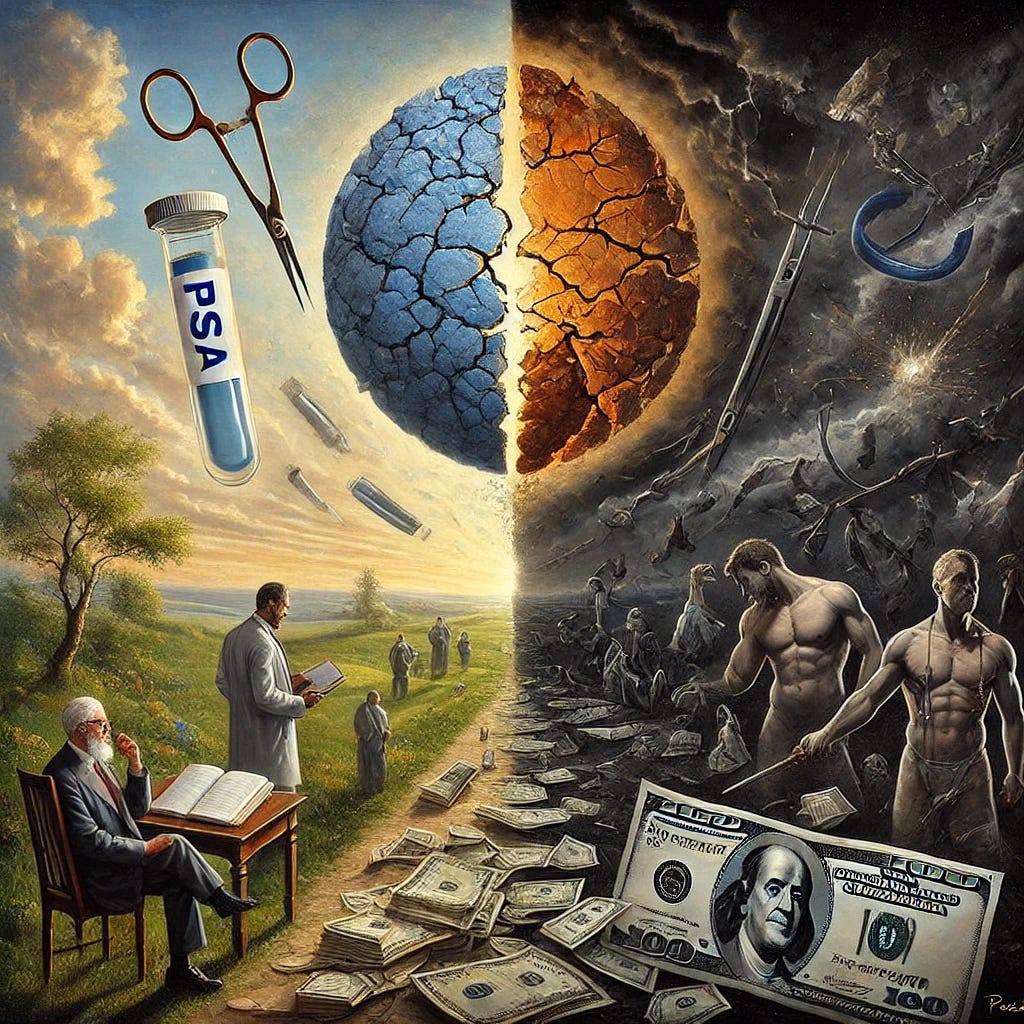
My most read stack of the last 3 years has been my summary of Ablin and Piana’s book.
The Great Prostate Hoax - Lies are Unbekoming
Radical prostatectomy, a common treatment resulting from PSA screening, often leads to significant side effects. Up to 60-80% of men experience erectile dysfunction and 10-20% have long-term urinary incontinence.
The PSA test has a high false-positive rate of up to 80%, leading to many unnecessary biopsies and treatments.
The predation here is especially synergistic as the maiming and destruction caused by prostate interventions feed two sub-Cartels, those of erectile dysfunction and incontinence. The adult diaper business is thriving because of this butchery. The urologists, not wanting to be left behind by pediatricians, cardiologists, dermatologists and dentists have their own cozy racket.
The prostate cancer racket is not discussed enough, and so I’m summarizing a second book.
With thanks to Dr Anthony Horan.
Let’s start with an analogy.
Analogy
Imagine you live in a small town where everyone owns cars. One day, a group of successful auto repair shops introduces a new diagnostic test that claims to identify potentially catastrophic engine failures before they happen. The test is heavily marketed and becomes routine in annual car maintenance.
The test frequently shows "concerning results" in older cars, even though most of these cars run perfectly well. When the test comes back positive, car owners are strongly encouraged to undergo complete engine replacements at significant cost. Local repair shops invest in expensive new equipment, mechanics receive special training, and the complete engine replacement becomes a major industry in town.
However, there's a crucial catch: Later analysis reveals that:
The test mainly detects normal engine wear that comes with age
For every 380 "concerning" test results, only one engine would have actually failed
Most importantly, many cars that get complete engine replacements already have tiny, undetectable issues in their transmissions and other systems that the engine replacement doesn't address
The expensive procedure often creates new problems: electrical system issues, transmission problems, and reduced performance
Some cars are actually damaged or destroyed by the unnecessary intervention
Older, more established repair shops in neighboring towns are much more hesitant to recommend engine replacements
This situation continues for years until a government agency finally declares that the testing does more harm than good. By then, thousands of car owners have undergone expensive, unnecessary engine replacements that often created more problems than they solved, while making the repair shops and equipment manufacturers very wealthy.
Just as a car is a complex system where problems in one area often indicate systemic issues, prostate cancer is typically a systemic disease that can't be "cured" by just removing the prostate. The PSA test, like our hypothetical engine test, created an epidemic of overtreatment that generated massive profits while often harming patients without extending their lives.
The story is ultimately about how financial incentives in medicine can transform a flawed diagnostic test into an industry that prioritizes profits over patient welfare, supported by a system that suppresses negative evidence while promoting profitable procedures.
12-point summary
For those that don’t want the deeper dive Q&A below.
In 1983, prostate cancer treatment shifted from a conservative, systemic approach to aggressive surgical intervention, peaking in 1992 with 2,815 excess deaths from radical prostatectomy. This change wasn't driven by scientific advancement but by financial opportunities.
PSA testing fundamentally lacked reliability as a screening tool, with a discovery-to-mortality ratio of 380:1. It correlated more strongly with benign enlargement than cancer, yet became the primary driver of unnecessary treatments.
Medicare/Medicaid legislation created a profit-driven medical system where hospitals earned approximately $16,990 per operation. The total industry revenue exceeded $1 billion, transforming prostate cancer into a major profit center.
Prostate cancer is characteristically slow-growing, with a doubling time of 475 days and approximately 52 years from first cancer cell to death. Most critically, it becomes metastatic at just 2mm diameter, long before detection is possible.
Treatment rates varied dramatically by region and social class. Wealthy, educated areas like Manhattan showed lower rates of radical surgery, while western states demonstrated significantly higher rates, revealing how cultural and social factors influenced medical decisions.
Treatment complications were severe and widespread, including 11,260 cases of urinary incontinence, with 8% of these patients experiencing suicidal thoughts. Sexual dysfunction affected both patients and partners, fundamentally altering quality of life.
Scientific evidence suffered from systemic publication bias, with negative findings often suppressed while positive results were prominently featured. This created a distorted picture of treatment effectiveness.
Research revealed prostate cancer's systemic nature, with 54-90% of patients showing cancer cells in bone marrow before surgery. This evidence fundamentally challenged the logic of localized treatments.
Institutional approaches varied significantly. The Veterans Administration showed remarkable restraint, while academic centers aggressively promoted surgery. The British system maintained a more conservative approach than the American system.
Patient quality of life considerations were often overlooked in the drive for treatment, despite evidence of significant physical and psychological impacts from aggressive interventions.
The 2012 U.S. Preventive Task Force statement marked a turning point, leading to a 26% drop in screening rates and a 35% decline in radical prostatectomies in some regions.
Future directions emphasize more selective testing, increased focus on systemic treatments, and a return to conservative management for low-risk disease, reflecting a renewed emphasis on evidence-based medicine over profit-driven care.
The Rise and Fall of the Prostate Cancer Scam (2019)
Dr Anthony Horan
40 Questions & Answers
How did prostate cancer treatment methodology change between 1973 and the 1990s, and what drove these changes?
In 1973, urologists had a clear approach to prostate cancer - no screening, no radiation, and no radical surgery. All discovered cancers were assumed to be metastatic from the beginning, and if treatment was necessary, it involved systemic hormone deprivation. This changed dramatically between 1983-1987 when radical surgery was revived without new scientific evidence. The introduction of miniaturized ultrasound probes for rectal examination and the PSA blood test catalyzed an epidemic of screening and treatment, despite PSA's documented lack of specificity for screening purposes.
The medical-industrial complex drove these changes through financial incentives. Medicare/Medicaid money poured into U.S. hospitals and faculty practice plans, creating a profitable industry around prostate cancer treatment. This shift wasn't based on scientific advancement but rather on economic opportunities, leading to an epidemic of over-diagnosis and over-treatment that peaked in 1992 with post-radical surgery deaths reaching 2,600.
What fundamental problems exist with PSA testing as a screening tool for prostate cancer?
PSA testing fundamentally lacks sufficient sensitivity and specificity to be an effective screening tool. When plotted on a receiver-operator curve, PSA testing with an action value of 4.0 ug/ml shows sensitivity versus specificity equivalent to flipping a coin. PSA levels correlate more strongly with benign prostatic hypertrophy (BPH) volume than with cancer, particularly in levels below 10 ng/ml, making it an unreliable indicator of cancer presence.
Moreover, PSA testing led to massive over-diagnosis of clinically insignificant cancers. The ratio of discovered cancers to those that would actually cause death was 380:1 for men over 50 years old. This means for every 380 prostate cancers present in autopsies, only one would have caused death, demonstrating how PSA testing created an epidemic of unnecessary treatment for non-lethal cancers.
Why did geographic variations in radical prostatectomy rates exist across different regions of the United States?
Geographic variations revealed stark cultural and socioeconomic patterns in treatment approaches. In Fresno, California, the radical prostatectomy rate was five times that of Manhattan, despite both cities having similar cultural amenities. The western states showed consistently higher rates of radical surgery compared to the Northeast, with Alaska's rate being twenty-one times that of Rhode Island's. This variation correlated strongly with social indicators such as teenage pregnancy, suicide rates, and auto accidents.
These differences reflected deeper sociological patterns. Areas with lower income and education levels had higher frequencies of radical prostatectomy, while wealthy, educated regions like Manhattan and San Francisco showed more restraint. The Northeast, with its older universities more committed to science, maintained lower rates than more recently founded medical schools in other regions. This geographic disparity highlighted how social class and cultural factors, rather than pure medical science, drove treatment decisions.
How did Medicare/Medicaid legislation in 1965 transform medical practice and influence prostate cancer treatment?
The 1965 Medicare/Medicaid legislation created a "tragedy of the commons" where cost control became irrelevant, particularly when cancer was involved. The legislation established a "usual and customary" fee structure without clear definitions or limits. This system allowed for virtually unlimited billing for "reasonable and necessary" treatments, creating a financial incentive for aggressive intervention rather than conservative management.
This transformation fundamentally altered medical practice economics. Faculty practice plans began generating massive revenues, and hospitals became dependent on Medicare/Medicaid money. The financial incentives created by this system encouraged the adoption of radical prostatectomy and other aggressive treatments, regardless of their proven efficacy. This shift from science-based medicine to profit-driven care fundamentally changed how prostate cancer was managed in the United States.
What evidence exists regarding bone marrow testing and its relationship to prostate cancer metastasis?
Bone marrow testing revealed crucial evidence about prostate cancer's systemic nature. Studies showed that 54% to 90% of patients had detectable cancer cells in their bone marrow prior to radical prostatectomy, using various detection methods. These findings were consistently demonstrated across multiple studies using increasingly sophisticated detection techniques, including monoclonal antibodies and polymerase chain reactions.
This evidence fundamentally challenged the rationale for radical surgery or radiation as curative treatments. The presence of cancer cells in bone marrow before local treatment indicated that the disease was already systemic at diagnosis, making local therapy alone insufficient for cure. However, this evidence was often downplayed or ignored because it threatened the profitable industry of radical prostatectomy and radiation therapy.
Statistics and Data Points
Prostate Cancer Natural History
Average doubling time: 475 days
Time from first cancer cell to death: 52 years
Cancer becomes metastatic at 2mm diameter
Mean time to death from incidental cancer discovery: 17.5 years (± 1.8 years)
Mortality and Complications
2,815 excess deaths from radical prostatectomy (1984-1998)
11,260 cases of post-surgical urinary incontinence
924 deaths from transrectal biopsy complications
Post-operative death rate quadrupled for age group over 75
Treatment Disparities
Fresno's radical prostatectomy rate was 5x higher than Manhattan's
Alaska's rate was 21x higher than Rhode Island's
Only 4% of British urologists would choose radical prostatectomy for themselves vs 79% of American urologists
Medicare collections for hospital and urologist services exceeded $1 billion
Cancer Detection
Ratio of discovered to lethal cancers: 380:1 in men over 50
54-90% of patients had detectable cancer cells in bone marrow before surgery
PSA testing had specificity of only 0.3 (70% false positives)
Hospital charge per radical prostatectomy: $16,990
Treatment Changes
26% drop in PSA screening (2010-2013) after USPTF statement
35% decline in radical prostatectomies after 2012
Percentage of low-risk patients receiving radical prostatectomy dropped from 42% (1994-1999) to 13% (2014-2015)
VA system showed only twofold increase in surgeries vs 6-7x increase in Medicare system (1986-1996)
How do mortality statistics reveal problems with radical prostatectomy as a treatment option?
Mortality statistics exposed significant issues with radical prostatectomy through several key metrics. The procedure resulted in approximately 2,815 excess deaths within thirty days of surgery between 1984 and 1998. This mortality spike was particularly evident in 1992, when prostate cancer death rates jumped from 22 to 25 per 100,000 in California, coinciding with the peak of radical prostatectomy procedures.
These deaths were often obscured by being scattered across time and geography, making them less visible than singular catastrophic events. The mortality rate was especially high in the elderly population, where the procedure quadrupled the baseline death rate for the age group. This data revealed that radical prostatectomy not only failed to extend life but actually increased mortality risk, particularly in older patients.
What role did financial incentives play in the adoption of various prostate cancer treatments?
Financial incentives pervaded every aspect of prostate cancer care. Medicare reimbursement policies made radical prostatectomy highly profitable, with hospitals receiving approximately $16,990 per operation. The total collections for hospital and urologist services reached over $1 billion in the peak years. Equipment manufacturers also profited substantially, with ultrasound equipment sales to urologists reaching approximately $219 million.
These financial motivations influenced treatment recommendations and practice patterns. Faculty practice plans paid more to physicians who performed more procedures, and hospitals benefited from facility fees. The system created a self-perpetuating cycle where economic interests, rather than scientific evidence, drove treatment decisions. Even when evidence emerged questioning the value of aggressive treatments, the financial incentives continued to influence practice patterns.
How does benign prostatic hypertrophy (BPH) relate to PSA levels and cancer diagnosis?
BPH fundamentally confounds PSA testing because it causes PSA elevation through mechanical pressure on prostate ducts. The relationship between BPH and PSA is direct and proportional - as BPH volume increases, PSA levels rise predictably. This means that many "elevated" PSA readings actually reflect BPH rather than cancer, leading to unnecessary biopsies and subsequent over-diagnosis of clinically insignificant cancers.
The mechanical relationship between BPH and PSA creates a critical flaw in using PSA as a cancer screening tool. For example, a 75-year-old man with 70cc's of BPH would normally have a PSA of 8.0, yet this level would trigger cancer concerns under standard protocols. This fundamental misunderstanding led to countless unnecessary biopsies and treatments, as doctors failed to account for the normal PSA elevations caused by BPH.
Why did the Veterans Administration approach prostate cancer treatment differently than the private sector?
The Veterans Administration (VA) system demonstrated greater restraint in adopting aggressive treatments because it operated under different financial incentives. As a capitated, government HMO, the VA had no financial motivation to perform unnecessary procedures. The nationwide increase in radical prostatectomies was less than twofold in the VA system from 1986 to 1996, compared to a six-to-seven-fold increase in the Medicare system.
The VA's approach reflected a more scientific, evidence-based methodology. Under the leadership of K. Kizer, M.D., the VA system emphasized counseling sessions before PSA testing and recognized the lack of evidence for life extension through screening and aggressive treatment. This systematic difference highlighted how removing profit motives led to more conservative, evidence-based treatment approaches.
What specific complications arise from radical prostatectomy and how frequently do they occur?
Radical prostatectomy produced severe complications beyond the immediate mortality risk. Approximately 11,260 cases of urinary incontinence occurred during the epidemic period, with 8% of incontinent patients experiencing suicidal ideation. Sexual dysfunction affected both patients and their partners, with studies showing significant reductions in quality of life for both. Additionally, 19% of patients experienced penile shortening of one to two centimeters.
The psychological impact of these complications was profound. Depression and anxiety were common, affecting both patients and their relationships. The procedure also led to cognitive impairment in elderly patients due to low blood pressure and anemia during surgery. These complications were often downplayed in the medical literature, demonstrating another aspect of publication bias in prostate cancer treatment.
How did publication bias affect prostate cancer treatment protocols?
Publication bias systematically suppressed negative findings about prostate cancer treatments while promoting positive ones. Research showing problems with radical prostatectomy or questioning PSA testing often appeared in less prestigious journals, at early morning conference sessions, or remained unpublished. This bias created a false impression of treatment efficacy because studies showing poor outcomes or complications were less likely to be published or prominently featured.
The cost of publishing, approximately $2,500 in labor per article, meant that many negative results never reached publication. When negative findings did get published, they were often relegated to less visible venues or given less prominence. This systematic bias created a self-reinforcing cycle where treatments appeared more successful than they actually were, perpetuating aggressive treatment approaches despite lack of scientific support.
What is the significance of cancer doubling times in prostate cancer management?
Prostate cancer doubling time, averaging 475 days, reveals crucial information about disease progression and appropriate treatment timing. This prolonged doubling time, compared to 58 days for other common cancers, means that prostate cancer takes approximately 52 years from the first cancerous cell to death. This extended timeline questions the urgency of aggressive intervention.
The doubling time varies by location in the body: 33 days in lymph nodes, twice that in bone marrow, and fourteen times slower in the primary site. Understanding these different growth rates explains why bone marrow metastases often dominate end-stage disease and why localized treatments targeting only the prostate fail to address the systemic nature of the disease.
How did French deconstruction theory influence medical practice?
French deconstruction theory, introduced to American medicine through Johns Hopkins, undermined traditional scientific hierarchies in medical decision-making. This philosophical approach suggested that since words have no fixed meaning, science itself was merely a social construct used by Northwest Europeans to maintain power. This perspective challenged the traditional doctor-patient relationship and medical authority.
The theory's influence led to a more egalitarian approach to medical decision-making, where patient choice became paramount regardless of medical expertise. This shift contributed to the practice of presenting treatment "options" to patients without clear medical guidance, effectively transferring complex medical decisions to potentially uninformed patients and contributing to overtreatment.
What role did academic medical centers play in promoting certain treatments?
Academic medical centers became driven by financial incentives after Medicare/Medicaid legislation transformed their economics. Faculty practice plans began generating significant revenue from procedures, with some professors earning $400,000 annually from clinical fees. This financial pressure led academic centers to promote profitable procedures like radical prostatectomy, despite lack of scientific evidence supporting their efficacy.
These centers shifted from their traditional role as guardians of scientific medicine to becoming business enterprises focused on generating revenue. The pressure to maintain hospital profitability and faculty income led to the promotion of aggressive treatments, even when evidence suggested more conservative approaches might be more appropriate. This transformation fundamentally altered the role of academic medicine in treatment decisions.
How does the British approach to prostate cancer differ from the American approach?
The British approach demonstrated greater skepticism toward aggressive prostate cancer treatments, influenced by their nationalized healthcare system. While 79% of American urologists would choose radical prostatectomy for themselves, only 4% of British urologists would make the same choice. This stark difference reflected fundamental differences in healthcare delivery systems and financial incentives.
The British system, based on capitation rather than fee-for-service, removed financial incentives for aggressive treatment. Their Working Party acknowledged that apparent improvements in survival rates were likely due to lead time bias and length bias, not treatment effectiveness. This more conservative approach reflected a system focused on evidence-based medicine rather than profit-driven care.
What are the key differences between transrectal and perineal biopsy methods?
The transrectal biopsy approach, despite being newer and widely adopted, showed significant disadvantages compared to the older perineal method. Transrectal biopsies had higher infection rates, with 16-73% of patients experiencing bacteremia, and resulted in dangerous complications including sepsis and death. The approach required passing needles through fecal material before entering the prostate, creating inherent infection risks.
The older perineal approach demonstrated superior cancer detection rates and fewer complications. Studies showed that the perineal route detected significantly more carcinomas in both autopsy and prostatectomy specimens. However, the transrectal approach was widely adopted because it was easier to perform, required less skill, and generated more revenue through equipment sales and procedures.
How does androgen deprivation therapy work and what are its effects?
Androgen deprivation therapy works by lowering male hormone levels, causing approximately 80% of prostate cancer cells to commit suicide. This systemic approach acknowledges the metastatic nature of the disease and can extend life by about three years when administered early. The therapy can be achieved through various methods, from surgical castration to medical treatments like LHRF antagonists.
The therapy's effects include both benefits and drawbacks. While it effectively controls cancer growth, it can lead to cognitive changes, including reduced word recall but improved executive function. It also affects quality of life through various side effects, including potential cardiovascular complications. The therapy can be administered intermittently rather than continuously, providing periods of normal hormone levels and improved quality of life.
What impact did insurance companies have on treatment decisions?
Insurance companies significantly influenced treatment decisions through their reimbursement policies and coverage decisions. They often engaged in practices that complicated patient care, such as delaying payments to physicians or denying claims. These practices led to class action lawsuits, including one involving 950,000 physicians suing Aetna under the RICCO statute.
The insurance system's influence extended beyond individual treatment decisions to shape entire treatment protocols. The ability to bill insurance companies for procedures encouraged the adoption of aggressive treatments, while the complexity of insurance systems often made it difficult for physicians to provide more conservative, less profitable approaches to care.
How did the definition of "cure" evolve in prostate cancer treatment?
The definition of "cure" underwent significant distortion in prostate cancer treatment literature. While the plain meaning implies permanent resolution of disease, the medical establishment began using modified definitions such as "ten years without biochemical evidence of recurrence" or "fifteen years without recurrence." This redefinition served to justify aggressive treatments despite lack of true cure.
This evolution of the definition masked the reality that prostate cancer often takes decades to become lethal, with a median time to death of 22 years for PSA-discovered cancer. The modified definition of cure allowed treatments to appear more successful than they were, contributing to overtreatment while obscuring the natural history of the disease.
What were the specific findings of the Swedish and PIVOT trials?
The Swedish and PIVOT trials provided crucial evidence about radical prostatectomy's effectiveness. The Swedish study showed no difference in overall mortality at 12 years between surgery and observation groups. While it initially reported a 5% advantage in cancer-specific mortality at 12 years, this advantage disappeared by 15 years of follow-up.
The PIVOT trial similarly demonstrated no overall benefit from radical surgery versus observation. These findings were particularly significant because they represented rare randomized, controlled trials in prostate cancer treatment. However, both trials were complicated by the fact that the surgery groups often received earlier androgen deprivation therapy, potentially confounding the results.
How did the US Preventive Task Force's 2012 statement impact prostate cancer care?
The USPTF's 2012 declaration that PSA-based screening caused more harm than good created a seismic shift in prostate cancer care. In Massachusetts, screening rates dropped 26% in ages 55-69 between 2010-2013. Other regions showed varying responses, with states like Alabama and Alaska showing 7.5% drops while Utah showed virtually no change, demonstrating the geographic variations in medical practice response to scientific evidence.
This statement triggered a 35% decline in radical prostatectomies and fundamentally changed treatment patterns. The percentage of low-risk disease patients receiving radical prostatectomy dropped from 42% in 1994-1999 to 13% in 2014-2015. The impact extended to radiation therapy businesses and led to financial losses for companies like Theragenics, highlighting how scientific evidence could overcome entrenched financial interests.
What role do systemic therapies play in prostate cancer treatment?
Systemic therapies recognize and address the whole-body nature of prostate cancer. Early chemotherapy combined with androgen deprivation showed significant survival benefits, with docetaxel demonstrating life extension of 17 months when combined with androgen deprivation in high-volume disease. Other systemic approaches include statins, aspirin, and metformin, which showed various degrees of effectiveness in cancer control.
Immunotherapy emerged as another promising systemic approach, with treatments like Sipuleucel-T showing survival benefits. The development of these systemic approaches represented a return to the pre-1983 understanding that prostate cancer is fundamentally a systemic disease requiring whole-body treatment rather than just localized intervention.
How did Bradford Walker, M.D.'s approach exemplify ideal medical practice?
Bradford Walker exemplified ideal medical practice through his patient-focused, non-commercial approach to medicine. Practicing in Cornwall, Connecticut, for over 50 years, he maintained the oldest active medical license in the state and demonstrated unwavering commitment to patient care rather than profit. His approach emphasized clinical judgment and patient welfare over financial considerations.
Walker's practice style contrasted sharply with modern commercialized medicine. He would visit patients after hospital rounds, maintained no public relations agenda, and focused solely on patient needs. His approach represented the pre-Medicare era of medicine where physician judgment and patient care took precedence over financial considerations and administrative pressures.
What were the economic implications of radical prostatectomy for hospitals and physicians?
Radical prostatectomy generated substantial revenue streams for both hospitals and physicians. Hospitals received approximately $16,990 per operation, while physicians collected around $1,849 per procedure under Medicare. The total collections for hospitals and urologists during the epidemic period reached over $1 billion, demonstrating the massive financial scale of this treatment approach.
These economic incentives created a self-perpetuating system where financial interests drove treatment decisions. Academic medical centers particularly benefited, with faculty practice plans generating significant revenue that supported other departments. This financial structure made it difficult to challenge the prevalence of radical prostatectomy, even when evidence questioned its effectiveness.
How did patient autonomy affect treatment decisions?
Patient autonomy, while seemingly empowering, often led to problematic treatment decisions. The practice of presenting patients with treatment "options" without clear medical guidance effectively transferred complex medical decisions to potentially uninformed patients. This approach, influenced by French deconstruction theory, assumed patients could make sophisticated medical decisions despite lacking medical training.
This shift toward patient autonomy paradoxically served the medical-industrial complex's interests. Patients, influenced by optimism and aggressive marketing, often chose more aggressive treatments than medical evidence would support. The concept of patient choice became a means of promoting more expensive, aggressive treatments while appearing to respect patient autonomy.
What role did pharmaceutical companies play in treatment protocols?
Pharmaceutical companies significantly influenced treatment protocols through medication pricing and marketing strategies. Companies like TAP Pharmaceuticals and AstraZeneca competed aggressively in the androgen deprivation therapy market, with medications like Lupron and Zoladex generating hundreds of millions in sales. Some companies engaged in questionable practices, including providing free samples that were then billed to Medicare.
The influence extended beyond direct drug sales to shaping treatment protocols. Companies marketed expensive hormone therapies aggressively, contributing to the shift toward medical rather than surgical castration despite cost differences. This pharmaceutical influence added significant costs to prostate cancer treatment while not necessarily improving outcomes.
How did medical education reforms affect prostate cancer treatment?
Medical education reforms, particularly following the Flexner Report, initially established scientific medicine as the foundation of medical practice. However, the introduction of Medicare/Medicaid funding transformed medical education by creating financial pressures that emphasized revenue generation over scientific rigor. This shift led to a decline in basic science faculty and an increase in clinical faculty focused on generating practice revenue.
The changes also included more elective courses and less required urology rotation time, with the percentage of medical schools requiring urology rotation dropping from 80% to 20% between the 1960s and 1990. This educational shift reduced exposure to urological principles and contributed to less critical evaluation of prostate cancer treatments.
What impact did social class have on treatment decisions and outcomes?
Social class significantly influenced prostate cancer treatment patterns. Higher-income, better-educated populations in areas like Manhattan and San Francisco showed lower rates of radical prostatectomy, while lower-income regions demonstrated higher rates. This pattern suggested that education and social class affected the ability to critically evaluate treatment options.
The correlation between social indicators and treatment choices revealed that cultural and economic factors, rather than pure medical science, often drove treatment decisions. Areas with higher education levels and more sophisticated medical communities tended to be more conservative in their treatment approaches, demonstrating how social class influenced medical decision-making.
How did lead time bias affect perceived treatment success?
Lead time bias created a false impression of treatment success by making it appear that early detection and treatment extended survival. When cancers were discovered earlier through PSA screening, patients appeared to live longer from diagnosis, even though the actual course of disease remained unchanged. This statistical artifact was often misrepresented as treatment success.
This bias significantly affected how treatment outcomes were reported and understood. The five-year survival rates touted by the American Cancer Society reflected earlier diagnosis rather than actual life extension. Understanding this bias was crucial for evaluating the true effectiveness of various treatments and screening approaches.
What were the specific complications of transrectal biopsies?
Transrectal biopsies carried significant risks, including severe infections and death. Between 16% and 73% of patients experienced bacteremia, with some developing serious complications like sepsis. An estimated 924 deaths occurred from transrectal biopsy complications during the epidemic period, with about 600 of these deaths occurring in patients whose biopsies were negative for cancer.
The complication rate was worsened by increasing antibiotic resistance and the inherent risks of passing needles through fecal material. Despite these risks, the procedure became widespread due to its ease of performance and financial incentives, even though the older perineal approach showed better safety profiles and cancer detection rates.
How did immunotherapy develop as a treatment option?
Immunotherapy for prostate cancer evolved from early observations of immune responses following cryosurgery. The freezing of prostate tissue occasionally triggered immune responses that affected distant metastases, suggesting potential systemic benefits. This led to the development of more sophisticated approaches like Sipuleucel-T, which uses the patient's own immune cells to target prostate cancer.
Modern immunotherapy developments include vaccines like PROSTVAC and immune checkpoint inhibitors. However, these treatments faced significant regulatory and financial hurdles. Dendreon's bankruptcy after developing Provenge demonstrated how regulatory requirements and pricing issues could impede immunotherapy advancement, even when treatments showed promise for extending survival.
What role did the American Urological Association play in treatment protocols?
The American Urological Association (AUA) attempted to balance scientific evidence with clinical practice through policy statements and guidelines. Their 1995 policy statement acknowledged the lack of high-quality evidence for many prostate cancer treatments, rating them as "options" rather than proven therapies. However, when translating these policies to public information, the AUA often failed to clearly convey the uncertainty surrounding treatment effectiveness.
The organization's influence extended to residency training requirements, where programs could be jeopardized if they didn't perform enough radical prostatectomies. This created pressure to maintain surgical volumes even as evidence questioned the procedure's value, demonstrating how professional organizations could perpetuate treatments despite scientific uncertainty.
How did the Flexner Report influence medical practice and education?
The Flexner Report fundamentally transformed American medical education by establishing scientific medicine as the foundation of medical practice. It led to the closure of two-thirds of medical schools and established standards requiring full-time faculty supported by endowments rather than clinical fees. This initially created a system where medical decisions were based on science rather than financial considerations.
However, the introduction of Medicare/Medicaid funding ultimately undermined Flexner's reforms by creating financial pressures that emphasized revenue generation over scientific rigor. The original vision of physicians supported by endowments gave way to faculty practice plans dependent on clinical revenue, fundamentally altering the relationship between medical education and clinical practice.
What were the key differences between university hospitals and private practice approaches?
University hospitals, despite their academic missions, often promoted more aggressive treatments due to financial pressures from faculty practice plans and hospital operations. These institutions needed to generate significant revenue to support their educational missions, leading them to favor profitable procedures like radical prostatectomy despite questionable evidence for their effectiveness.
Private practitioners, particularly in solo practice, often faced different pressures. While they needed to maintain financial viability, they weren't subject to the same institutional pressures as university hospitals. However, they were influenced by insurance reimbursement policies and the need to maintain referral relationships, which could affect treatment recommendations.
How did publication practices affect treatment protocols?
Publication practices systematically favored positive results about aggressive treatments while suppressing negative findings. Studies showing problems with radical prostatectomy or questioning PSA testing often faced significant hurdles to publication, including harsh peer review from referees who had financial interests in maintaining current treatment patterns.
This bias created a self-reinforcing cycle where treatments appeared more successful than they actually were. The cost of publishing and the preference for positive results meant that complications, negative outcomes, and treatment failures were underrepresented in the medical literature, distorting the evidence base for treatment decisions.
What role did chemotherapy play in prostate cancer treatment?
Chemotherapy's role evolved from a last-resort treatment to an earlier intervention option, particularly when combined with androgen deprivation therapy. The CHAARTED study demonstrated significant survival benefits when docetaxel was administered early in treatment, especially for high-volume disease, extending survival by 17 months.
The timing of chemotherapy proved crucial, with early administration showing better results than waiting until hormone therapy failed. However, the treatment carried significant risks, including bone marrow failure, requiring careful patient selection and monitoring. The development of new chemotherapy protocols represented a return to viewing prostate cancer as a systemic disease requiring systemic treatment.
How did patient narratives influence understanding of treatment outcomes?
Patient narratives, particularly from well-known writers and intellectuals, provided crucial insights into treatment experiences and outcomes. These accounts, from figures like Cornelius Ryan, Max Lerner, and others, revealed the personal impact of various treatments and often highlighted problems that weren't adequately captured in medical literature.
However, these narratives sometimes created misconceptions about typical disease progression. For example, accounts of aggressive cancers that progressed quickly could distort understanding of the typically slow-growing nature of most prostate cancers, potentially encouraging more aggressive treatment approaches than necessary.
What were the specific effects of radiation therapy and its complications?
Radiation therapy demonstrated significant complications while failing to provide clear survival benefits. It increased bladder cancer risk threefold and could cause devastating complications including fistulas between the urinary tract and rectum. The therapy often led to more aggressive cancer behavior by causing sublethal injury to cancer cell DNA.
The treatment's effects extended beyond immediate complications to include delayed problems appearing 5-10 years after treatment. These included secondary cancers, urinary problems requiring hyperbaric oxygen treatment, and progressive arterial damage leading to erectile dysfunction. The therapy's carcinogenic effects often escaped documentation due to the extended time between treatment and complications.
How did quality of life considerations affect treatment decisions?
Quality of life considerations became increasingly important as evidence emerged about treatment complications. Sexual function, urinary continence, and overall well-being were significantly affected by aggressive treatments. Studies showed that both patients and their partners experienced reduced quality of life following radical treatments, with some patients experiencing depression and suicidal thoughts.
Despite these concerns, quality of life considerations often took a back seat to the drive for "cure." The medical system's focus on treating cancer sometimes overshadowed the impact of treatments on patients' daily lives, leading to situations where treatments caused more immediate suffering than the disease itself.
What recommendations emerged for future prostate cancer treatment approaches?
Future treatment recommendations emphasized a more nuanced, evidence-based approach. These included careful consideration of PSA testing modifications, increased use of PSA density measurements, and more selective use of biopsies. The approach recognized the need to distinguish between aggressive cancers requiring intervention and indolent cancers that could be safely monitored.
Systemic treatments gained prominence, with recommendations for earlier use of androgen deprivation therapy and chemotherapy in appropriate cases. The focus shifted toward identifying truly high-risk patients while avoiding overtreatment of low-risk disease, representing a return to more conservative management approaches based on scientific evidence rather than financial incentives.
I appreciate you being here.
If you've found the content interesting, useful and maybe even helpful, please consider supporting it through a small paid subscription. While everything here is free, your paid subscription is important as it helps in covering some of the operational costs and supports the continuation of this independent research and journalism work. It also helps keep it free for those that cannot afford to pay.
Please make full use of the Free Libraries.
Unbekoming Interview Library: Great interviews across a spectrum of important topics.
Unbekoming Book Summary Library: Concise summaries of important books.
Stories
I'm always in search of good stories, people with valuable expertise and helpful books. Please don't hesitate to get in touch at unbekoming@outlook.com
For COVID vaccine injury
Consider the FLCCC Post-Vaccine Treatment as a resource.
Baseline Human Health
Watch and share this profound 21-minute video to understand and appreciate what health looks like without vaccination.




In 1993, my cousin called me and said the doctors told him he had 3 months to live because he had prostate cancer. Being in the drug business, he wanted to know if I could get him a discount on an expensive drug to treat it sold by Schering. I gave him a phone number to call. Ten years later he called me. I said: George! You are suppose to be dead! What happened? George said: I joined a self help group and I have been taking 10,000 iu's of Vitamin D daily! I said: You are poisoning yourself! I was told by the professor that taught us at the pharmacy school that taking more than 1000 iu's daily was a poison. TOTAL LIE! All medical professionals since WWII have been told this lie! Since 2009, when I meet the founder of www.grassrootshealth.net I have learned the truth about the true value of Vitamin D and I now know the active form is essential in turning on about 3000 gene expressions when required. One of the gene expressions is the production of E-Cadherin which is a special protein that surrounds cancer cells and prevents metastasis! To this day, Big Medicine and Big Pharma ignore the true value of Vitamin D because it will negatively impact their profitable medical business. The VA in the USA ran a test and gave veterans in a few Midwest locations Vitamin D as a normal regimen. It reduced overall medical appointments by about 50%. THEY IGNORED THEIR OWN RESEARCH AND DEEP SIX'D THE PROGRAM! You don't grow the bureaucracy that way. My thoughts for the day. thomasabraunrph@substack.com
I am closing in on 75 and never had a PSA test and never will. I am 100% sure I'll die of something but I have no confidence or trust in the medical profession to save me from anything.