Is Psychiatry a Crime Against Humanity? (2024)
By Peter C. Gøtzsche – 40 Q&As – Unbekoming Book Summary
In truth, I had underestimated just how vile psychiatry truly is, and I’m actively working to correct that.
I’m open to being corrected, but it seems to me that vaccination marked the first instance of "industrial-scale corruption," followed by oncology, driven by Flexner and the creation of the AMA under Rockefeller’s influence, with psychiatry trailing closely behind.
While reviewing and summarizing this book, the penny finally dropped about the “chemical imbalance” myth—I had unquestionably fallen for that one.
Gøtzsche is a big deal and he paid special attention to psychiatry in this book:
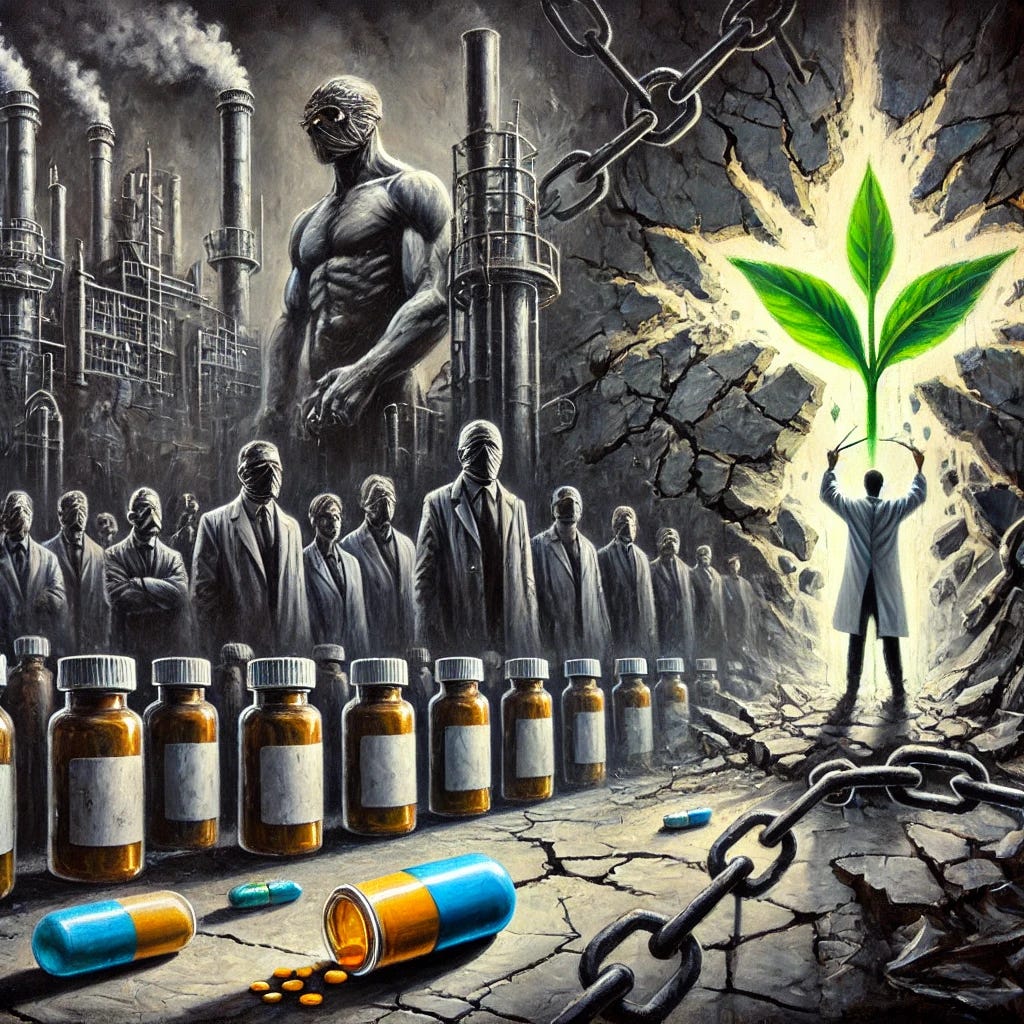
Peter C. Gøtzsche's book, "Is Psychiatry a Crime Against Humanity?" is a scathing critique of modern psychiatry, challenging its core principles and practices. Gøtzsche argues that the field is built upon a foundation of harmful myths, particularly the chemical imbalance theory, which he contends is a marketing ploy to push psychiatric drugs. He criticizes the widespread use of these medications, claiming they are rarely necessary, often ineffective, and carry a high risk of serious side effects, including addiction, suicide, and death.
The book meticulously deconstructs common beliefs about psychiatric treatments, including the notion of easy withdrawal from antidepressants and the idea that these drugs improve long-term outcomes. Gøtzsche exposes the myth of antipsychotic benefits, arguing that they can shrink the brain and may not improve long-term outcomes for patients. He highlights the dangers of overdiagnosis and overmedication, fueled by the pharmaceutical industry's influence. The book champions a more humane, patient-centered approach, advocating for psychotherapy and other non-drug therapies, informed consent, and an end to forced treatment. Ultimately, "Is Psychiatry a Crime Against Humanity?" calls for a radical transformation of mental health care based on scientific evidence, ethical principles, and respect for patients' rights.
With thanks to Peter C. Gøtzsche.
Related
Podcast Conversation (3 Book Discussion)
Analogy
Imagine a car repair industry where mechanics are trained to believe that all cars have fundamental engineering defects that require permanent chemical additives in the fuel system. Instead of examining why a car isn't running properly - perhaps it needs basic maintenance, better fuel, or has a specific fixable problem - these mechanics immediately add chemical substances to the fuel tank that alter the engine's basic functioning.
These additives make the engine run more slowly and less efficiently, often damaging vital components over time. When car owners try to stop using these additives, their engines sputter and stall even worse than before, which the mechanics claim "proves" the owners need the additives forever. The mechanics insist this is the only proper way to maintain cars, despite clear evidence that cars run better without these chemicals and that simple mechanical repairs or regular maintenance would solve most problems.
To make matters worse, the companies making these fuel additives fund all the mechanic training schools, write the repair manuals, and suppress evidence of engine damage. They also pay the most prominent mechanics to promote their products and discredit anyone who suggests cars might run better without chemical additives.
This is modern psychiatry: instead of addressing the real causes of human distress and offering genuine help, it forces people onto harmful drugs that create the very problems they claim to treat, while suppressing evidence of damage and punishing those who speak out against this practice.
Just as cars don't need harmful chemical additives but rather proper maintenance and specific repairs when problems arise, humans experiencing mental distress need genuine support, understanding, and practical help - not brain-altering drugs that create dependency and cause long-term harm.
My Most Important Advice to Patients
Usually, only a few people hold extreme views, but in psychiatry, the vast majority believe in a specialty built on myths, lies, and flawed research. This is very harmful for patients. You will learn more about this in the following chapters.
Therefore, even though there are exceptions, as a precaution, if you have a mental health issue, you should not see a psychiatrist. It is dangerous and might turn out to be the biggest error of your life. Any contact with psychiatry is likely to lead to treatment with one or more psychiatric drugs that will harm you.
I have heard numerous stories from patients with a common theme. They had no idea how dangerous it was to become a psychiatric patient and trusted their doctors, until they found out many years later that their lives had been ruined.
I shall also warn against seeing a family doctor. As doctors are trained to use drugs, you will most likely be harmed. It is better to find someone who is good at talk therapy, e.g. a psychologist or psychotherapist, and if there is a long waiting list, it is usually better to do nothing.
Since you cannot trust what doctors tell you about mental health issues and psychiatric drugs, you might want to look up the evidence yourself. It is much easier than you might think. If a doctor writes a prescription for a psychiatric drug, don’t go to the pharmacy. Go on the Internet and find the officially approved package insert, e.g. by writing Prozac FDA package insert. If you read it, you’ll likely know more about the drug than your doctor does. I am not joking. If doctors knew what is written in package inserts, they wouldn’t prescribe so many drugs.
When you have read the package insert, you might decide not to take the drug. Psychiatric drugs are very rarely needed, and if so, only in acute situations, never long-term. You can also find much useful information on the Internet, but it requires quite some understanding of research methodology to be able to judge if what you find is reliable.
Peter C. Gøtzsche
12-point summary
1. Drug Ineffectiveness: Psychiatric drugs lack meaningful clinical effectiveness. Depression pills show minimal difference from placebo (2 points on Hamilton Scale where 5-6 points is minimum noticeable), antipsychotics lack long-term benefits, and ADHD medications show no benefits after three years.
2. Mortality Impact: Psychiatric drugs are the third leading cause of death after heart disease and cancer. Depression pills double suicide risk across all age groups, and antipsychotics kill 1-2 patients per 100 treated for just ten weeks in dementia patients.
3. Diagnosis Unreliability: Psychiatric diagnoses show poor reliability between clinicians. Studies demonstrate that most healthy people can be diagnosed with mental illness when tested, and diagnostic criteria are arbitrary and lacking scientific validity.
4. Chemical Imbalance Myth: The chemical imbalance theory of mental illness has been thoroughly debunked. No evidence supports claims of serotonin deficiency or other chemical imbalances causing mental health problems, despite this remaining a common justification for medication.
5. Research Fraud: Widespread fraud exists in psychiatric research. Companies routinely hide negative results, manipulate data, and publish positive results multiple times under different authors' names. The STAR*D study exemplifies this, claiming 67% success while actual remission rate was 3%.
6. Industry Influence: Pharmaceutical industry profoundly influences psychiatric practice through financial relationships with leading psychiatrists, funding of professional organizations, control of research data, and marketing campaigns disguised as education.
7. Withdrawal Effects: Psychiatric drug withdrawal can be severe and long-lasting. Studies show 56% of patients experience withdrawal symptoms, with 25% having severe effects. Symptoms can persist for years and are often misinterpreted as relapse.
8. Forced Treatment: Forced psychiatric treatment violates human rights and leads to worse outcomes. Studies show closer contact with psychiatric services increases suicide risk, and forced treatment often traumatizes patients.
9. Long-term Outcomes: Long-term studies consistently show better outcomes for patients who discontinue psychiatric drugs compared to those maintained on them. Studies found better recovery rates in countries with low medication use.
10. Alternative Approaches: Psychosocial interventions consistently show better outcomes than medication. Exercise, psychotherapy, and Open Dialogue approach demonstrate superior results without medication's risks.
11. Children's Vulnerability: Psychiatric drugs particularly harm children. ADHD medications stunt growth by 5cm after 16 years, depression pills double suicide risk, and long-term studies show worse outcomes for medicated children.
12. System Reform Needs: Fundamental reform of psychiatric practice is needed, including ending forced treatment, establishing withdrawal support services, prioritizing psychosocial interventions, and removing most psychiatric drugs from the market.
The Myth of Chemical Imbalance
Psychiatrists invented the myth of a chemical imbalance to motivate patients to take psychiatric drugs.
Psychiatrists claim that mental disorders like depression are caused by low serotonin, schizophrenia by high dopamine, and ADHD by low dopamine.
Psychiatrists compare taking psychiatric drugs to taking insulin for diabetes, which is a false equivalence.
There is no scientific evidence to support the claim that a chemical imbalance in the brain causes mental disorders.
Depression is not a result of a faulty brain, but a normal brain responding to stress or adversity.
Mental disorders are strongly associated with social, economic, and physical environments, including poverty, violence, and discrimination.
Many psychiatrists continue to propagate this myth despite scientific evidence debunking it.
Most psychiatric textbooks published from 1990 to 2010 supported the chemical imbalance hypothesis.
A 2019 study of popular websites in 10 countries found that 74% of websites attributed depression to a chemical imbalance or claimed that drugs could correct such an imbalance.
Patients often feel they cannot stop taking their drugs because they have been led to believe the chemical imbalance myth.
Statistics
Psychiatric drugs are rarely needed and only for acute situations, never long-term.
Contact with psychiatry is likely to lead to treatment with one or more psychiatric drugs that can be harmful.
A study including 71 clinical study reports and 18,426 patients showed that 12% more patients dropped out while on a psychiatric drug than on a placebo, suggesting that the drugs are even worse than reported.
The quality of life data reporting in the clinical study reports from this study was virtually non-existent.
Only 3% of the patients who entered the STAR*D trial for depression remitted, stayed well, and stayed in the trial during the one-year follow-up.
Duloxetine increases the risk of suicide and violence 4-5 times in middle-aged women with urinary incontinence.
There is no study that shows psychiatric drugs improve long-term outcomes, and all long-term studies demonstrate serious drug harms.
The CATIE trial, which randomized 1493 patients with schizophrenia, found that after 18 months only 26% of the patients were still on the drug.
It has been known for 70 years that psychiatric drugs worsen negative symptoms and cognition.
In the 10-year follow-up TIPS study of 281 patients with first-episode psychosis, 12% of patients died although their average age was only 29 years old.
About half of the patients in the TIPS study would have developed tardive dyskinesia and many, if not all, would have developed permanent brain damage after 10 years.
Stimulants double the risk of cardiovascular events.
Involuntary hospital admissions in Europe range from 12 per 100,000 in Italy to 233 per 100,000 in Finland.
A recent survey showed that only 1% of New Zealanders on depression pills had been told anything about withdrawal effects or addiction.
A median of 50% of the patients succeeded in withdrawing from their depression pills in a study of withdrawal.
40 Questions & Answers
Question 1: What does research reveal about psychiatric drug effectiveness compared to marketed claims?
Studies consistently show that psychiatric drugs are far less effective than marketed claims suggest. For depression medications, the difference between drug and placebo is only 2 points on the Hamilton Scale, where the smallest perceivable effect is 5-6 points. Network meta-analyses and systematic reviews repeatedly fail to show clinically relevant effects. The landmark STAR*D study, costing $35 million, found only 3% of patients remained well after one year on medication. In placebo-controlled trials, the evidence shows that more patients drop out while on drugs than on placebo, indicating patients find the harms outweigh any perceived benefits.
Industry-sponsored studies routinely overstate benefits while understating harms. Even when effects are claimed to be statistically significant, they have no real-world relevance. Documentation shows that companies selectively publish positive results while suppressing negative ones, creating a distorted picture of effectiveness. The actual clinical impact of these medications falls far below the thresholds that would indicate meaningful improvement in patients' conditions, yet marketing continues to promote them as highly effective treatments.
Question 2: What are the mortality risks associated with psychiatric drug use?
Psychiatric drugs are the third leading cause of death after heart disease and cancer, with particularly severe impacts on vulnerable populations. Depression medications double suicide risk across all age groups, with studies showing especially high risks in people under 25 years old. The rate of suicidal events is shockingly high - 2 out of 100 young people experienced suicidal events during just a few weeks of treatment in clinical trials. These risks persist throughout treatment and are particularly elevated during any dose changes.
Antipsychotics show especially concerning mortality rates, killing one to two per hundred dementia patients treated for about ten weeks. Overall mortality for schizophrenia patients has increased markedly, with standardized mortality ratios rising from 1.84 in the 1970s to 3.20 in the 1990s, coinciding with increased use of newer antipsychotic drugs. The elderly face particularly high risks, with studies showing that about one in five elderly patients die within a year after a psychiatric drug-related hip fracture.
The Myths of Psychiatry
The Myth of Chemical Imbalance:
The book argues that the idea of mental disorders being caused by chemical imbalances in the brain is a myth perpetuated by psychiatrists to encourage patients to take drugs.
Gøtzsche asserts that there is no scientific basis for this claim and that mental disorders are complex and likely stem from a combination of genetic predispositions and life experiences.
He criticizes the comparison of psychiatric drugs to insulin for diabetes as a misleading oversimplification.
The Myth of Easy Withdrawal:
The book dispels the myth that stopping treatment with antidepressants is easy.
It emphasizes that withdrawal from psychiatric drugs can be challenging and may cause various side effects, including psychological and physical discomfort.
The Myth of Psychiatric Drugs as Cure-alls:
The book argues against the idea that psychotropic drugs for mental illness are akin to insulin for diabetes.
Gøtzsche highlights that, unlike insulin, psychiatric drugs do not address the underlying causes of mental disorders and may not provide long-term benefits.
He contends that the emphasis on drug treatment has led to the neglect of other potentially beneficial therapies, such as psychotherapy.
The Myth of Reduced Chronicity:
The book challenges the myth that psychotropic drugs reduce the number of chronically ill patients.
It presents evidence suggesting that long-term use of psychiatric drugs can lead to dependence and worsen the overall prognosis for many patients.
Gøtzsche argues that this approach has contributed to an increase in the number of people receiving disability payments for mental disorders.
The Myth of Safety:
The book debunks the myths that antidepressants are safe and non-addictive.
It provides evidence that antidepressants can increase the risk of suicide in children and adolescents and have other serious side effects.
Gøtzsche emphasizes that psychiatric drugs are the third leading cause of death and should be used with extreme caution.
The Myth of Antipsychotic Benefits:
The book criticizes the claim that antipsychotics prevent brain damage and reduce the risk of death in patients with psychoses.
Gøtzsche cites studies showing that antipsychotics can shrink the brain and may not improve long-term outcomes for patients.
He argues that the widespread use of antipsychotics has led to unnecessary harm and suffering for many patients.
The Myth of Untreated Mental Illness:
The book argues against the myth that the main problem in psychiatry is undertreatment rather than overtreatment.
Gøtzsche presents evidence that many people are being diagnosed and treated for mental disorders that they do not have and that this overdiagnosis and overtreatment are causing significant harm.
He criticizes the influence of the pharmaceutical industry in promoting the expansion of diagnostic criteria and the overuse of psychiatric drugs.
Other Myths:
The book also addresses myths regarding specific treatments, such as the effectiveness of electroconvulsive therapy (ECT) and the benefits of psychosurgery.
It highlights the dangers of involuntary treatment in psychiatry and advocates for a more humane and patient-centered approach to mental health care.
This list provides a summary of the key myths addressed in the book. The book offers detailed explanations and evidence to support these claims.
Question 3: How do psychiatric drugs affect brain structure and function?
Psychiatric drugs create permanent changes in brain function by disrupting normal neurotransmitter systems, leading to lasting alterations in neural pathways and cognitive processes. Studies show that antipsychotics shrink the brain in a dose-dependent manner, while antidepressants can cause permanent sexual dysfunction, cognitive impairment, and emotional blunting. These medications impair higher brain functions including thinking, feeling, memory, and empathy, often creating deficits that persist even after discontinuation.
The changes in brain structure and function are not limited to temporary effects during treatment but can persist long after medication is stopped. Research demonstrates that these drugs fundamentally alter neural plasticity and neurotransmitter receptor sensitivity, leading to compensatory changes in brain circuitry. The result is often a cascade of adaptations that can make it difficult or impossible for the brain to return to its original state, even after the medication is discontinued.
I've said for years the only way to get through grief and depression is to Go Through It! You can't bury or cover it up or fix it with drugs, ever. I lost a baby years ago due to placental abruption and was inconsolable so the doc gave me some valium to 'help me'. Well it worked and I was happy, smiling, and laughing until I realized I HAD A REASON TO BE DEPRESSED AND GRIEVING...and I tossed those pills in the garbage and just let myself feel my loss. I did the same when my best friend passed, when my mother died, when my husband died. It is normal to hurt and grieve deeply with loss, and for that pain to resurface at times throughout the rest of our lives. Grief and its depression is NOT linear, it ebbs and flows through life, and it shapes how we handle nearly everything in our lives. - DNPmom
Question 4: What are the specific effects of long-term antipsychotic use?
Long-term antipsychotic use causes severe physical and neurological damage that accumulates over time, with studies showing that patients maintained on these drugs have worse outcomes than those who discontinue them. These medications cause tardive dyskinesia in approximately 4-5% of patients per year of use, meaning most long-term users will eventually develop this often irreversible movement disorder. Brain scans reveal progressive tissue loss in multiple regions, and patients experience increasing cognitive difficulties with continued use.
The drugs also cause serious metabolic problems, diabetes, and cardiovascular disease at rates far higher than the general population. WHO studies found that patients in developing countries where antipsychotic use was low had much better recovery rates than those in developed countries with high usage rates. Long-term users die on average 15-20 years earlier than the general population, with mortality increasing in proportion to the duration and dose of medication.
Question 5: How do ADHD medications impact children's development?
ADHD medications demonstrably stunt children's physical growth and development, with research showing that children who consistently took stimulants were 5cm shorter after 16 years compared to those who took very little. The drugs suppress children's spontaneous mental and behavioral activity, reduce social interest, and can cause depression, compulsive behaviors, and personality changes. Animal studies confirm these behavioral changes and suggest potential permanent effects on brain development.
The MTA study, which cost $35 million, revealed that by years six to eight, medicated children had worse ADHD symptoms and were more functionally impaired than those not taking medication. Additionally, contrary to claims that these medications prevent substance abuse, research shows they actually increase the risk of later substance use problems. The drugs provide no long-term benefits while potentially creating permanent alterations in brain development and behavior.
Question 6: What are the characteristics and prevalence of psychiatric drug withdrawal?
Withdrawal from psychiatric drugs affects up to 56% of patients, with 25% experiencing severe withdrawal effects that can persist for months or years. Common symptoms include akathisia (severe internal restlessness), anxiety, depression, insomnia, and psychosis. A significant study found that in 16% of cases, withdrawal symptoms lasted over three years, demonstrating the long-term impact these drugs can have even after discontinuation. These effects are frequently misinterpreted as relapse, leading to inappropriate resumption of drug use.
The withdrawal process is particularly challenging because symptoms often emerge or worsen when patients attempt to reduce their medication, creating a cycle of dependency. Surveys indicate that many patients make multiple attempts to discontinue their medications before succeeding, with some ultimately unable to stop due to severe withdrawal effects. The psychiatric establishment has historically minimized or denied these withdrawal effects, leaving patients without proper support or understanding of their experiences.
I was prescribed Prozac 30 years ago for stress related insomnia. The insomnia has long gone but I’ve given up trying to stop taking this drug. The withdrawal effects are horrific! I’ve resigned myself to being on it for life 😢. - Marie
Question 7: How can psychiatric drug withdrawal be safely managed?
Safe withdrawal from psychiatric drugs requires an extremely slow tapering process due to the hyperbolic binding curves of these medications. The process typically takes months or years, with dose reductions becoming progressively smaller over time to minimize withdrawal effects. Success requires careful monitoring and support systems, including access to compounding pharmacies or liquid formulations to allow for minute dose adjustments, particularly in the final stages of withdrawal.
Individual responses to withdrawal vary significantly, necessitating personalized approaches rather than standardized protocols. Support systems are essential, including knowledgeable practitioners, withdrawal clinics, and peer support networks. The most challenging period often comes during the final small reductions, where even tiny changes in dose can produce significant effects. Many patients require specialized formulations or compounding to achieve the very small doses needed for the final stages of withdrawal.
Question 8: What barriers exist to successful withdrawal?
The psychiatric establishment's persistent denial or minimization of withdrawal effects creates significant barriers to successful discontinuation of these medications. Many practitioners misinterpret withdrawal symptoms as relapse, pressuring patients to resume full dosage rather than supporting careful tapering. The lack of withdrawal clinics and limited insurance coverage for tapering support leaves many patients attempting to withdraw without proper medical supervision or guidance.
The hyperbolic binding curve of psychiatric drugs means that standard tapering schedules are usually too rapid, yet few practitioners understand this pharmacological principle. Patients often face skepticism or hostility from healthcare providers when requesting support for withdrawal, and many are told they need to remain on medication for life. The lack of professional understanding and support, combined with limited access to appropriate tapering tools and formulations, makes successful withdrawal unnecessarily difficult for many patients.
Question 9: How does industry funding affect psychiatric research?
Industry funding profoundly influences research outcomes through multiple mechanisms that systematically bias results in favor of drug treatment. Industry-funded trials are far more likely to report positive results than independent studies, with research showing this effect is not due to better methodology but rather to selective reporting and data manipulation. Companies control access to trial data, allowing them to hide negative results while publishing positive ones multiple times under different authors' names, creating a false impression of consistent benefits.
The influence extends beyond direct trial funding to shape entire research agendas and methodologies. Companies design trials to maximize chances of showing benefit while minimizing detection of harms, using techniques such as exclusion criteria, short duration studies, and selective outcome measures. Department chairs and leading researchers often receive substantial payments from drug companies, creating systemic bias that affects study design, data interpretation, and publication decisions. This web of financial relationships creates a research environment where negative findings are suppressed and positive results are amplified.
Our daughter was groomed to prozac in the public high school counselor (partnering with a 3rd party therapist but dedicated to the high school), recruited to participate in LGBTQ programming and then lost the opportunity to participate in the Air Force when she graduated due to being on Prozac. She tried to get off the drug for her senior year with no success. She continued on the drugs after high school, made really sad life choices by moving from the midwest to L.A. to have a rough life. 6 years later, still on the drugs, not able to get her life together. She has alienated herself from our family, very sad. - Sw
Question 10: What are common flaws in psychiatric research methodology?
Psychiatric research methodology suffers from fundamental flaws that systematically overestimate benefits while underestimating harms. Most trials are short-term studies with ineffective blinding due to obvious drug side effects, yet they're used to justify long-term treatment. They typically exclude patients who improve on placebo during initial run-in periods or include only those who have previously tolerated the drug, creating biased samples that don't represent real-world patients. Outcome measures rely heavily on subjective rating scales rather than meaningful life outcomes.
The methodology routinely ignores withdrawal effects when comparing drugs to placebo, as most patients entering trials are already taking psychiatric drugs that are abruptly discontinued if they're assigned to the placebo group. This creates withdrawal effects in the placebo group that are misinterpreted as evidence of drug efficacy. Studies often use "enriched" designs that pre-select patients who respond well to the drug while excluding those who don't tolerate it, artificially inflating apparent effectiveness. These methodological choices consistently produce results that overstate benefits while minimizing or hiding harms.
Question 11: How prevalent is research fraud in psychiatric drug trials?
Research fraud is endemic in psychiatric drug trials, with numerous documented cases of deliberate data manipulation and suppression of negative findings. A prime example is Study 329 of paroxetine, where GlaxoSmithKline claimed the drug was safe and effective while knowing both claims were false. The study was negative for all eight protocol-specified outcomes, but the company manipulated the data to appear positive. Similar fraud has been documented in trials of other medications, where adverse events including suicide attempts were systematically omitted from publications.
The fraud extends beyond individual studies to create systematic distortion of the evidence base. Companies routinely hide negative trial results while publishing positive ones multiple times under different authors' names. The STAR*D study, costing $35 million, represents another major fraud where investigators claimed a 67% remission rate while careful analysis showed only 3% of patients who entered the trial remitted and stayed well during the follow-up year. Over 100 papers were published from this study, all maintaining the false narrative of treatment success.
Question 12: How do regulatory bodies oversee psychiatric drug approval?
Regulatory bodies consistently fail to protect public safety, instead serving industry interests through various mechanisms of compromised oversight. The FDA has repeatedly suppressed information about suicide risks and prevented safety officers from presenting negative findings to advisory committees. When reviewing suicide risk in 2006, they allowed companies to self-report adverse events rather than conducting independent analyses, effectively allowing the industry to hide serious safety problems.
The European Medicines Agency and other regulators have similarly failed in their oversight duties, approving drugs based on flawed evidence and accepting trials with major methodological problems. When confronted with evidence of problems, these agencies often delay action or make minimal changes while allowing dangerous practices to continue. The revolving door between industry and regulatory agencies creates conflicts of interest that compromise the integrity of the approval process, leading to decisions that prioritize commercial interests over public safety.
Question 13: What role do academic institutions play?
Academic institutions actively protect and perpetuate harmful psychiatric practices despite mounting evidence of problems. Universities often cover up research misconduct, protect researchers with industry ties, and suppress criticism of conventional practices. Department chairs routinely receive industry "discretionary funds" that they can use as they please, creating systemic conflicts of interest that influence research priorities and training programs. These institutions frequently prevent critical research from being published while promoting industry-friendly narratives about psychiatric drugs and diagnoses.
The academic environment is particularly hostile to reform efforts, with critics and reformers often facing professional retaliation for questioning conventional practices. Universities depend heavily on industry funding for research and educational programs, creating institutional resistance to any challenges to drug-based psychiatry. Faculty who attempt to reduce medication use or question conventional practices often face marginalization, loss of resources, and barriers to publication, effectively suppressing alternative approaches and maintaining the status quo.
Question 14: How does the pharmaceutical industry influence prescribing practices?
Drug marketing directly drives prescription patterns, with usage increasing in direct proportion to marketing efforts rather than clinical need. Companies employ sophisticated strategies targeting both doctors and the public through paid key opinion leaders, sponsored education events, and direct-to-consumer advertising where allowed. They create new diagnostic categories to expand markets and promote the idea that normal life experiences require drug treatment, leading to massive overprescription for increasingly minor conditions.
The industry exerts particular influence through financial relationships with prescribers, with psychiatrists collecting more money from drug companies than doctors in any other specialty. Those who receive the most money tend to prescribe more medications, particularly to vulnerable populations like children. Companies create marketing campaigns disguised as education, funding professional organizations and continuing medical education programs that promote drug use while downplaying risks and alternatives.
Question 15: How do psychiatric textbooks present information?
Psychiatric textbooks consistently misrepresent scientific evidence, presenting false or misleading information about drug benefits while minimizing or ignoring harms. They promote unproven biological theories of mental illness, make unsupported claims about drug effectiveness, and ignore evidence of serious adverse effects. Many textbooks continue to promote the debunked chemical imbalance theory and make false claims about the long-term safety and efficacy of psychiatric drugs, despite clear evidence to the contrary.
This distorted presentation creates a system where new psychiatrists are indoctrinated with false beliefs that harm patients. Textbooks often omit or minimize information about withdrawal effects, deny drug dependency issues, and present psychiatric diagnoses as more reliable than research shows. Industry influence on textbook content is significant, with many books being ghost-written or authored by individuals with substantial industry ties. This creates a self-perpetuating cycle where each new generation of practitioners is trained to maintain harmful practices.
Question 16: How does the psychiatric guild protect its interests?
The psychiatric guild maintains control through systematic suppression of criticism, control of professional organizations, and attacks on reformers who challenge conventional practices. Critics are often labeled as "anti-psychiatry" regardless of their credentials or the evidence they present. Professional organizations like the American Psychiatric Association and Royal College of Psychiatrists consistently defend harmful practices while attacking those who question them, maintaining their authority through control of training, certification, and publication venues.
Those who challenge conventional practices often face professional ostracism, loss of positions, and attacks on their credibility. The guild works actively to prevent reforms that might reduce drug use or challenge biological psychiatry's dominance, using its influence over professional training and certification requirements to maintain the status quo. This creates a self-perpetuating system where challenging conventional wisdom becomes professionally dangerous, effectively suppressing innovation and reform.
Question 17: What role do patient advocacy groups play?
Many prominent patient advocacy groups have been compromised by pharmaceutical industry funding, leading them to promote drug treatment while downplaying risks and alternatives. These organizations often receive substantial financial support from drug companies, creating conflicts of interest that influence their messaging and advocacy positions. For example, MIND, an influential UK mental health charity, refused to publish advertisements for drug withdrawal courses despite many members seeking such help. These groups frequently perpetuate false narratives about chemical imbalances and the necessity of long-term medication.
However, some genuine grassroots patient organizations work effectively to expose psychiatric harm and promote alternatives, facing significant challenges from the psychiatric establishment and industry-funded groups. These independent organizations often provide crucial support for those attempting to withdraw from psychiatric drugs or seeking non-drug treatments. They face ongoing challenges from better-funded industry-aligned groups that work to discredit their efforts and maintain the status quo of drug-based treatment.
Question 18: How are patient rights protected or violated in practice?
Despite theoretical legal protections, psychiatric patients often face systematic violations of basic human rights, particularly through forced treatment and coerced medication compliance. Patients are routinely drugged against their will and subjected to mechanical restraints, even when capable of making informed decisions about their care. Documentation shows widespread violation of existing legal protections, with a review of 30 consecutive cases from one Psychiatric Appeals Board finding that the law had been violated in every single case.
The system provides little meaningful recourse for patients who have been harmed or whose rights have been violated. When patients report adverse effects from medications, these are often labeled as symptoms of their underlying condition rather than drug effects. Complaints about forced treatment or rights violations are frequently ignored or dismissed through claims that patients lack insight into their illness. Even when patients present clear evidence of harm, their experiences are often discounted, and attempts to pursue legal remedies face significant obstacles.
Question 19: How does forced treatment affect outcomes?
Forced psychiatric treatment often traumatizes patients and leads to worse outcomes, with studies showing that involuntary treatment increases suicide risk. Research demonstrates a marked dose-response relationship: the closer the contact with psychiatric staff, the greater the risk of suicide. A Danish register study of 2,429 suicides showed that patients admitted to hospital had the highest risk, and this finding was robust even when accounting for illness severity. The use of force destroys trust between patients and healthcare providers, making future voluntary treatment unlikely.
Many patients subjected to forced treatment develop post-traumatic stress disorder and may avoid seeking help in the future, even when experiencing serious distress. Patients frequently report that forced treatment feels like rape or torture, particularly when it involves forced injections or physical restraints. This trauma can persist long after the immediate treatment ends, creating lasting barriers to accessing healthcare. Studies show that services can operate successfully without using force when adequate support is provided, demonstrating that coercive practices often reflect staff convenience rather than clinical necessity.
Question 20: How do patients experience psychiatric treatment?
Psychiatric survivors consistently report experiences of dehumanization, loss of autonomy, and iatrogenic harm from treatment. Many describe having their personalities fundamentally altered by psychiatric drugs, losing their ability to feel emotions or maintain relationships. Patients frequently report being told they have chemical imbalances requiring lifelong medication, only to discover later that this was false. Their attempts to discontinue medications are often met with hostility or threats, and many experienced severe adverse effects that were dismissed or denied by their doctors.
The impact on daily life is often severe, with patients reporting that psychiatric drugs make it difficult or impossible to work, maintain relationships, or enjoy normal activities. Common themes in patient accounts include being stigmatized by diagnoses, having valid concerns dismissed as symptoms, and suffering permanent harm from treatments. Those who successfully withdrew often found their original problems were manageable without drugs, but they had lost years or decades of their lives to psychiatric treatment. Many report that their attempts to communicate about adverse effects or withdrawal symptoms were met with disbelief or accusations of non-compliance.
Question 21: How does psychiatric treatment affect families?
Psychiatric treatment often places severe burdens on families while providing little genuine support or guidance. Families frequently report being given false information about the nature of psychiatric disorders and the effects of treatments, often being told their loved ones require lifelong medication while receiving no information about serious risks or alternatives. Many families have lost members to suicide or severe adverse effects while being told the treatments were protective. The system often uses families' concerns against patients, turning family members into enforcers of medication compliance rather than sources of support.
When patients experience adverse effects or wish to withdraw from medications, families often find themselves caught between conflicting information from practitioners and their own observations of harm. Many families report feeling betrayed when they later discover they were given false information about diagnoses and treatments. The burden of caring for family members experiencing drug adverse effects falls heavily on families, who often must navigate complex healthcare systems while watching their loved ones deteriorate under treatment. This creates lasting trauma and distrust of the mental health system among family members.
Question 22: How do psychiatric drugs affect quality of life?
Psychiatric drugs typically worsen quality of life through a combination of emotional blunting, cognitive impairment, and sexual dysfunction. They suppress normal emotional responses and social functioning, making it difficult for patients to experience normal pleasures or maintain relationships. Studies consistently show that more patients drop out of clinical trials while on drugs than on placebo, indicating that patients find the overall impact on their lives negative. Many patients report feeling like "zombies" or experiencing personality changes that affect their ability to work, maintain relationships, and enjoy life.
The drugs often create the very problems they claim to treat, leading to increased isolation and disability rather than recovery. Data shows that disability rates for mental health conditions have increased dramatically in parallel with increased psychiatric drug use. Sexual dysfunction affects up to 50% of patients taking antidepressants, with some experiencing permanent effects even after discontinuation. Cognitive impairment can persist long after stopping the medications, affecting memory, concentration, and emotional processing abilities.
Question 23: How reliable are psychiatric diagnoses?
Psychiatric diagnoses show remarkably poor reliability even among experienced clinicians, with major implications for treatment validity. In the largest reliability study of 592 people, agreement between psychiatrists was notably low, with kappa values of only 0.64-0.65 for major diagnoses like depression and schizophrenia. This means the difference between observed agreement and chance agreement is only 64% of the difference between perfect agreement and chance agreement. The diagnostic criteria are vague and arbitrary, with significant overlap between categories.
Studies demonstrate that most healthy people can be diagnosed with one or more mental illnesses if thoroughly evaluated. The number of patients diagnosed with schizophrenia has quadrupled in 40 years, demonstrating the unreliability of diagnostic practices. Screening tests for depression are so poor that for every 100 healthy people screened, 36 would receive a false depression diagnosis. This unreliability in diagnosis leads to inappropriate treatment and unnecessary medication of many individuals who may not have clinically significant conditions.
Question 24: How valid is the chemical imbalance theory?
The chemical imbalance theory, though thoroughly debunked by scientific research, continues to influence psychiatric care and public understanding of mental health. Despite no evidence supporting claims of serotonin deficiency or other chemical imbalances causing mental health problems, surveys show that 80% of patients believe their disorder is caused by chemical imbalances. This theory was primarily a marketing tool created and promoted by pharmaceutical companies to sell medications, yet it has become deeply embedded in both professional and public consciousness.
This false belief has made many patients reluctant to consider drug withdrawal, believing they need medications like diabetics need insulin. The theory has led to inappropriate prescribing, with normal emotional responses to life circumstances being treated as chemical deficiencies requiring drug intervention. Leading psychiatric authorities have admitted it was never more than a marketing tool, yet its influence persists, causing many patients to believe they have permanent brain defects requiring lifelong medication. This misconception often prevents people from exploring non-drug approaches or attempting to discontinue medications even when experiencing severe adverse effects.
Question 25: How effective are psychiatric screening tools?
Psychiatric screening tools produce alarmingly high rates of false positives, leading to overdiagnosis and unnecessary treatment. For depression screening, studies show that 36 out of 100 healthy people would receive false diagnoses when using standard screening tools. These instruments often pathologize normal responses to life circumstances, failing to distinguish between ordinary distress and clinically significant conditions. The widespread use of these tools in primary care and other settings contributes significantly to overdiagnosis and unnecessary medication of healthy individuals.
The validity of these screening tools is further compromised by their development and promotion by pharmaceutical companies seeking to expand their markets. Many screening questionnaires use arbitrary cutoff points that lack scientific validation, and their sensitivity and specificity values are often poor. The tools frequently ignore context and life circumstances, treating normal reactions to adverse events as symptoms of mental illness. This leads to medicalization of ordinary human experiences and contributes to the dramatic increase in psychiatric diagnoses and drug prescriptions.
Question 26: How do psychosocial interventions compare to medication?
Psychosocial interventions consistently demonstrate superior long-term outcomes compared to medication-based treatments. Studies show that psychotherapy halves the risk of suicide attempts while drugs double it, and exercise has shown substantial effects for depression, with studies finding only 30% of patients in exercise groups remained depressed compared to 52% in medication groups after six months. The Open Dialogue approach, which minimizes drug use and focuses on psychosocial support, shows dramatically better outcomes than traditional drug-based approaches, with only 19% of patients on disability allowance after five years compared to 62% of traditionally treated patients.
Research consistently demonstrates that psychological and social interventions provide more sustainable improvements without the risks associated with medication. Cognitive behavioral therapy shows large effects for anxiety disorders, and even paraprofessionals achieve similar results to professionals in providing psychological support. Support facilities providing 24-hour crisis care without compulsion effectively prevent hospitalization, while peer support groups show significant benefits without the risks of drug treatment. These approaches address underlying issues rather than merely suppressing symptoms, leading to better long-term outcomes.
Question 27: What factors influence treatment outcomes?
Treatment outcomes depend more heavily on the quality of therapeutic alliance between practitioner and patient than on whether treatment involves psychotherapy or drugs. WHO studies have consistently found better recovery rates in developing countries where drug use was low, suggesting that social support and community integration play crucial roles in recovery. The therapeutic relationship and the patient's belief in the treatment approach appear to be more significant factors than the specific intervention used.
Support systems and social factors play decisive roles in recovery outcomes. Research shows that patients with strong social networks and meaningful activities have better outcomes regardless of treatment type. Environmental factors, including stable housing, employment opportunities, and community acceptance, significantly influence recovery success. Studies demonstrate that addressing social determinants of mental health often produces better results than focusing solely on symptom suppression through medication.
Question 28: How effective are drug-free approaches?
Drug-free approaches often demonstrate superior outcomes to medication-based treatments across various conditions. The Open Dialogue program achieves remarkable results with minimal medication use, showing recovery rates far higher than conventional treatment. Exercise shows consistent benefits for depression, anxiety, and other conditions, with studies demonstrating effectiveness equal or superior to medication. Psychotherapy, particularly cognitive behavioral therapy, produces lasting improvements without the risks associated with drug treatment.
Support facilities providing crisis care without compulsion effectively prevent hospitalization while respecting patient autonomy. Peer support programs show significant benefits in helping people manage psychological distress and build coping skills. These approaches often address root causes of distress rather than merely suppressing symptoms, leading to more sustainable improvements. Research consistently shows that when drug-free alternatives are available and properly supported, many patients prefer them and achieve better outcomes than with medication-based treatment.
Question 29: What barriers exist to accessing alternatives?
Alternative treatments are often unavailable or not covered by insurance, despite evidence of their effectiveness. Patients seeking drug-free treatment frequently face long waiting lists or are told such approaches are dangerous, even when research supports their safety and efficacy. The system's focus on medication makes accessing alternative treatments particularly difficult for those with limited resources. Many practitioners lack training in non-drug approaches and may be skeptical or dismissive of patients' requests to explore alternatives.
Insurance systems often create significant financial barriers by limiting coverage for psychotherapy and other non-drug treatments while readily covering medications. The shortage of practitioners trained in alternative approaches, combined with limited institutional support for such programs, makes it difficult for many patients to access evidence-based non-drug treatments. These systemic barriers particularly affect vulnerable populations who may lack the resources to pay out-of-pocket for alternative treatments, effectively forcing them into medication-based approaches regardless of their preferences or needs.
Question 30: How do different countries approach psychiatric care?
Approaches to psychiatric care vary dramatically between countries, with striking differences in outcomes. WHO studies have consistently found much better recovery rates from psychosis in developing countries where drug use was low compared to developed countries with high medication use. European countries show enormous variations in forced treatment rates, ranging from 12 per 100,000 in Italy to 233 per 100,000 in Finland, demonstrating that many practices considered "necessary" in some countries are successfully avoided in others.
These international variations reveal that many harmful practices are cultural rather than necessary. Some countries have eliminated certain practices like electroshock therapy entirely, while others have developed successful programs that minimize drug use and coercion. The Open Dialogue approach in Finland and similar programs in other countries demonstrate that better outcomes are possible with reduced reliance on medication and force. These differences highlight the role of cultural and institutional factors in shaping psychiatric practice and challenge assumptions about the necessity of conventional drug-based approaches.
Question 31: What can be learned from successful alternative programs?
Programs like Open Dialogue in Finland demonstrate the possibility of achieving superior outcomes with minimal drug use and an emphasis on social support. These successful alternatives typically focus on early intervention, social network inclusion, and respect for patient autonomy. They achieve better recovery rates and lower levels of disability than conventional treatment while reducing or eliminating practices like forced treatment and long-term medication use. These programs show that many conventional psychiatric practices are not necessary for effective care.
The success of alternative programs highlights several key principles: the importance of preserving patients' social connections, the value of crisis support without coercion, and the benefits of minimizing drug use, particularly long-term medication. These approaches often cost less than conventional treatment while producing better outcomes. Their success challenges fundamental assumptions about the nature of mental health problems and their treatment, suggesting that many current practices may be counterproductive.
Question 32: What reforms are needed in psychiatric education?
Psychiatric education requires fundamental reform to break free from industry influence and biological reductionism. Training should emphasize psychosocial approaches, understanding trauma, and safe drug withdrawal rather than primarily focusing on medication management. Students need accurate information about drug risks and the lack of evidence for biological theories of mental illness. The influence of pharmaceutical funding on education must end, and students need exposure to critics of current practices and psychiatric survivors.
The curriculum must address the poor reliability of psychiatric diagnoses and the limitations of drug treatments. Future practitioners need training in providing genuine support rather than simply prescribing medications. Education should include comprehensive instruction about drug withdrawal effects and management, as well as extensive exposure to alternative treatment approaches. Reformed education must emphasize critical thinking and evidence-based practice while acknowledging the role of social factors in mental health.
Question 33: How can research quality be improved?
Research quality in psychiatry requires fundamental improvements including longer follow-up periods and focus on patient-relevant outcomes rather than short-term changes in rating scale scores. All trial data must be made publicly available, and studies must include treatment-naïve patients rather than those already on drugs. Independent funding and oversight are essential to eliminate industry bias, and negative results must be published alongside positive findings. Research must examine long-term outcomes and real-world effectiveness rather than just short-term efficacy in controlled settings.
Methodological improvements must include better attention to withdrawal effects, more meaningful outcome measures, and proper study of adverse effects. Research should prioritize patient-centered outcomes like quality of life, functional ability, and long-term well-being rather than symptom scores. Studies need to examine the full range of treatment approaches, including non-drug alternatives, and investigate factors that contribute to recovery. Publication bias must be eliminated through mandatory registration and reporting of all trials.
Question 34: What changes are needed in diagnostic practices?
Diagnostic practices require complete overhaul, moving away from arbitrary checklists toward understanding individual problems in their life context. The focus should shift from labeling to understanding specific problems and their causes, acknowledging the role of trauma, life circumstances, and social factors rather than assuming biological causes. Screening tools that produce high rates of false positives should be abandoned in favor of more comprehensive assessment approaches that consider context and individual circumstances.
The system must stop treating normal responses to life difficulties as medical disorders requiring drug treatment. New approaches should emphasize understanding the meaning and context of psychological distress rather than simply categorizing symptoms. Diagnostic practices need to acknowledge the role of social determinants of mental health and consider environmental factors that contribute to psychological distress. This requires moving beyond the current paradigm of discrete disorders toward a more nuanced understanding of human suffering and resilience.
Question 35: How can patient rights be better protected?
Patient rights protection requires legal reform to end forced treatment and ensure genuine informed consent. Independent advocacy services and legal representation must be readily available, and advance directives regarding treatment preferences should be legally binding. Oversight systems must be reformed to take patient complaints seriously and provide meaningful recourse for rights violations. Professional organizations and licensing bodies must enforce standards protecting patient autonomy.
Patients need protection from retaliation for refusing treatment or filing complaints. Systems must be established to ensure patients receive complete information about treatment risks and alternatives, and coercion through threats of involuntary commitment or loss of benefits must be eliminated. Meaningful accountability mechanisms must be created for practitioners and institutions that violate patient rights. Patient experience and testimony must be given proper weight in decision-making about treatment.
Question 36: How does polypharmacy affect outcomes?
Psychiatric drug polypharmacy (the use of multiple psychiatric drugs simultaneously) increases deaths without improving outcomes. Studies show that mortality increases with the number of antipsychotics prescribed, yet polypharmacy has increased dramatically, with office visits involving three or more drugs doubling in just nine years. The practice lacks scientific support but continues growing, driven by pharmaceutical marketing and the tendency to treat drug side effects with additional medications.
The combinations used in polypharmacy often involve drugs working against each other, like simultaneously prescribing medications that increase and decrease dopamine levels. This practice increases adverse effects and makes it more difficult for patients to discontinue medications. The complexity of drug interactions in polypharmacy makes it nearly impossible to determine which drugs are causing which effects, leading to cascading prescriptions where new drugs are added to counteract the effects of existing ones.
Question 37: What role does publication bias play?
Publication bias in psychiatric research is pervasive and systematic, with negative trials often going unpublished while positive ones are published multiple times under different author names. Studies showing drug harms are particularly likely to remain unpublished, and even fatal adverse events are often omitted from published papers. Analysis of clinical study reports reveals that important safety information is routinely withheld from publication, creating a distorted picture of drug benefits and risks.
When negative studies are published, they are often manipulated to appear positive through selective reporting of outcomes and statistical manipulation. Companies control access to trial data, allowing them to manage how results are presented in the literature. Multiple publication of positive results, often with slight variations in presentation or authorship, creates a false impression of consistent evidence supporting drug treatment. This systematic distortion of the evidence base makes it difficult for practitioners and patients to make informed decisions about treatment.
Question 38: How does psychiatric treatment affect disability rates?
Disability rates for mental health conditions have increased dramatically in parallel with increased psychiatric drug use, contrary to claims that these medications improve functional outcomes. Data shows that the expansion of drug treatment correlates with rising rather than falling disability rates. Long-term studies consistently show that patients maintained on psychiatric drugs have worse functional outcomes than those who discontinue treatment, suggesting that the medications may be contributing to rather than alleviating disability.
The drugs often create impairments that make it difficult for patients to work or function independently. Cognitive effects, emotional blunting, and physical side effects can make employment and normal activities challenging or impossible. WHO studies show better functional outcomes in countries with lower drug use, suggesting that intensive medication may be counterproductive for many patients. The shift toward long-term maintenance treatment appears to be contributing to increased chronicity and disability.
Question 39: What is the state of informed consent in psychiatry?
Despite theoretical requirements for informed consent, genuine informed consent rarely occurs in psychiatric practice. Patients receive incomplete or false information about risks and alternatives, often being told they have chemical imbalances requiring lifelong medication while receiving no information about serious adverse effects or alternative treatments. Coercion through threats of involuntary commitment or loss of benefits is common, making truly voluntary consent impossible for many patients.
Even when patients have advance directives or clearly stated treatment preferences, these are often overridden through claims of medical necessity or lack of insight. The system particularly fails to protect patients' rights to refuse treatment or to attempt drug withdrawal. Patients who express desire to reduce or stop medications often face threats or abandonment by their providers. Some lose custody of their children or face other social consequences for refusing psychiatric treatment, even when they are competent to make their own decisions.
Question 40: How can evidence-based reform be implemented?
Implementation of evidence-based reform requires fundamental changes to end industry influence on research and practice. The first priority must be establishing truly independent research funding and oversight to ensure studies focus on patient outcomes rather than commercial interests. Systems must be restructured to support psychosocial interventions that show better outcomes than drugs, including making these treatments readily available and covered by insurance. This requires breaking free from guild interests that maintain harmful practices despite evidence, and creating new accountability mechanisms for practitioners and institutions.
Successful reform requires changes at multiple levels: education reform to train practitioners in evidence-based approaches, policy changes to ensure patient access to alternative treatments, and systemic reforms to protect patient rights and autonomy. Key elements include establishing withdrawal clinics to support medication discontinuation, creating oversight bodies free from industry influence, mandating transparent reporting of all research results, and developing new practice guidelines based on patient outcomes rather than industry preferences. Public education about the limitations of current treatments and the availability of alternatives is also essential. These reforms must be supported by legal changes to end forced treatment and ensure genuine informed consent.
I appreciate you being here.
If you've found the content interesting, useful and maybe even helpful, please consider supporting it through a small paid subscription. While everything here is free, your paid subscription is important as it helps in covering some of the operational costs and supports the continuation of this independent research and journalism work. It also helps keep it free for those that cannot afford to pay.
Please make full use of the Free Libraries.
Unbekoming Interview Library: Great interviews across a spectrum of important topics.
Unbekoming Book Summary Library: Concise summaries of important books.
Stories
I'm always in search of good stories, people with valuable expertise and helpful books. Please don't hesitate to get in touch at unbekoming@outlook.com
For COVID vaccine injury
Consider the FLCCC Post-Vaccine Treatment as a resource.
Baseline Human Health
Watch and share this profound 21-minute video to understand and appreciate what health looks like without vaccination.




HERE IS A QUESTION TO ALL SHRINKS WORLDWIDE:
WHAT IS A NORMAL HUMAN LIKE?
BEFORE YOU ANSWER THIS, DO NOT APPROACH ANYBODY WITH YER FUCKED UP THEORIES ABOUT ABNORMAL BEHAVIOR.
ARROGANT, VAIN, GREEDY, POWER HUNGRY AND UNSCIENTIFIC SHITHEADS.
Yes, as is the entirety of the UNITED STATES INDUSTRIAL COMPLEX- Military, Pharmaceutical, Medical, Department of Education, etc.