Beyond Contagion
Rethinking "Pandemics" Through the Lens of Synchronized Biological Stress – by Denis Rancourt – 40 Q&As
The central message from my wonderful interview with Michael Allen Bryant could be summarized this way.
No Pandemic - Lies are Unbekoming
The history of disease is riddled with fraud, driven by economic and political agendas rather than public health. The HIV/AIDS crisis, for example, set the blueprint for modern 'health emergencies' like COVID-19: fear-driven narratives, manipulated data, and harmful treatments masquerading as solutions—all profiting a medical-industrial complex intertwined with global financial markets. Germ theory, foundational to modern medicine, obscures root causes like toxins, malnutrition, and social conditions, enabling a profitable cycle of 'treatments' over cures. The COVID-19 pandemic exemplified this, with questionable testing methods and policies that prioritized wealth transfer and control over health. Media and institutions like the WHO played pivotal roles, crafting narratives to justify draconian measures and entrench biosecurity states. Meanwhile, the elderly and vulnerable were collateral damage, sacrificed to protect failing economic systems. Ultimately, this isn't about health—it's about consolidating power and wealth under the guise of public safety.
Yes, there has been plenty of death, but it wasn’t a “virus” that caused it.
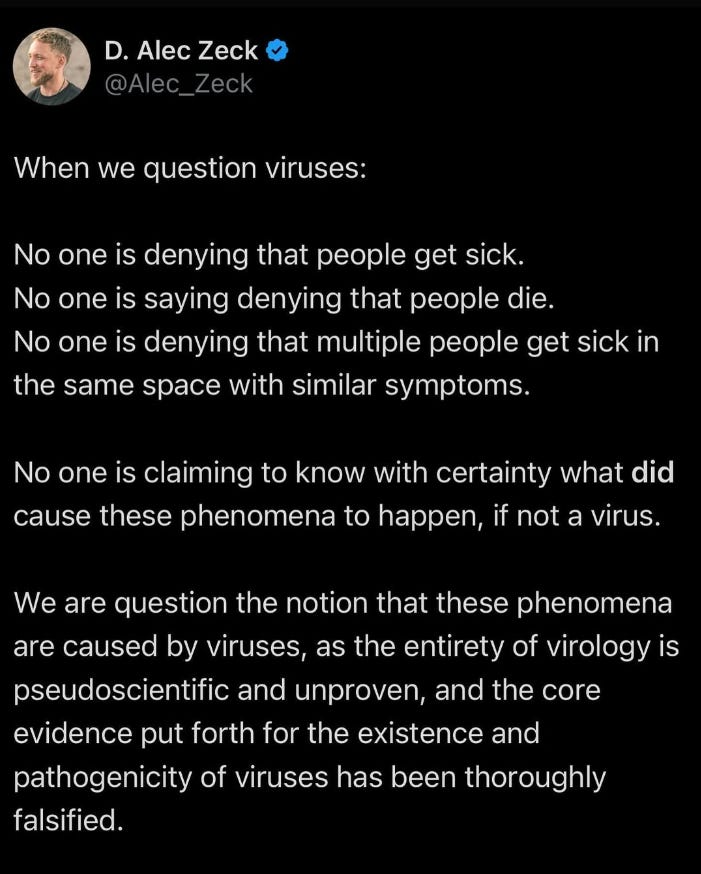
I’ve recently started to pay attention to D. Alec Zeck and I’m in tune with his thinking. This is a good summary of a position I now subscribe to.
The one and only Denis Rancourt has taken the conversation further with a 59-page medical hypothesis paper.
Medical Hypothesis: Respiratory epidemics and pandemics without viral transmission
It is worthy of amplification.
With thanks, as always, to Denis Rancourt.
Let’s start with an analogy.
Related work:
Italy 2020: Inside Covid’s Ground Zero
Analogy
Imagine a garden with many distinct plots in different neighborhoods. Each plot contains similar plants, but their health and survival depend primarily on local conditions - soil quality, water access, and care received - rather than on seeds traveling between gardens.
During times of widespread drought or when all gardeners simultaneously change their care methods (perhaps following new but misguided gardening protocols), plants across many gardens might wilt or die at the same time. While it might appear that a plant disease spread from garden to garden, the simultaneous decline actually results from similar stressful conditions affecting all gardens at once. The wealthier neighborhoods with better soil, irrigation systems, and resources to maintain proper care see their gardens remain healthier, while poorer areas with fewer resources experience more devastating effects.
This parallels the central argument: widespread health impacts during pandemics may not result from pathogens spreading between people, but rather from similar stressors (environmental, medical, or social) simultaneously affecting vulnerable populations. Just as plants carry their own potential for disease when stressed, humans harbor microbiomes that can become harmful under stressful conditions, particularly when deprived of proper care and resources.
12-point summary
Key Environmental Triggers: Environmental conditions, including temperature, atmospheric pressure, and humidity, directly affect respiratory health and can trigger synchronized disease patterns across populations without requiring pathogen transmission. This explains both seasonal mortality patterns and pandemic-scale health events.
Stress as Primary Driver: Biological and psychological stress function as fundamental causes of disease, particularly through immunosuppression and disruption of the respiratory tract microbiome. This can trigger simultaneous health impacts across populations exposed to similar stressors.
Medical Intervention Impact: Evidence shows strong temporal correlations between medical interventions (including mechanical ventilation, experimental treatments, and vaccination campaigns) and mortality peaks, suggesting these interventions played a significant role in excess deaths during 2020-2023.
Socioeconomic Influence: Social and economic factors strongly determine health outcomes, with clear evidence that position in social hierarchy and access to resources significantly affect mortality rates during health crises, independent of pathogen exposure.
Self-Generated Disease: Research demonstrates that serious respiratory conditions, particularly bacterial pneumonia, can develop spontaneously within individuals without requiring person-to-person transmission, especially in elderly and vulnerable populations.
Institutional Response Effects: Coordinated institutional responses, including lockdowns and treatment protocols, show strong temporal associations with mortality peaks across different regions, suggesting these responses themselves functioned as primary drivers of health outcomes.
Age-Related Vulnerability: Age exponentially increases vulnerability to stress-induced health impacts, particularly affecting respiratory systems. This explains why mortality patterns during health crises show strong age-dependent effects independent of pathogen exposure.
Care Home Conditions: Pre-existing conditions in care homes, including widespread malnutrition and dehydration, created baseline vulnerabilities that were exacerbated by pandemic responses, leading to significant mortality increases.
Diagnostic Impact: Changes in diagnostic practices and testing protocols influenced treatment decisions and mortality classifications, creating feedback loops that affected health outcomes rather than merely recording them.
Historical Patterns: Evidence from historical pandemics, including medieval plagues and volcanic-related health crises, supports the theory that environmental and socioeconomic factors, rather than pathogen transmission, drive pandemic-scale health events.
Geographic Correlations: Strong correlations exist between mortality patterns and geographic factors, particularly latitude and environmental conditions, without evidence of spread between regions, supporting environmental rather than transmission-based mechanisms.
Microbiome Role: Current understanding of the respiratory tract microbiome shows how stress and environmental changes can trigger rapid shifts from healthy to pathogenic states without requiring external pathogens, providing a mechanism for synchronized respiratory disease outbreaks.
40 Questions & Answers
1. What key evidence challenges the viral transmission theory of the 2020-2023 COVID-19 pandemic?
Major incompatibilities exist in the spatiotemporal mortality patterns, particularly during March-May 2020, where mortality peaks occurred simultaneously in various locations rather than showing viral spread patterns. The data shows no evidence of mortality peaks crossing national borders or having delayed effects in adjacent regions, which would be expected with viral transmission. About 30% of countries showed no detectable excess mortality until vaccine rollouts began, contradicting viral spread theory.
Large country-to-country heterogeneity in age and frailty adjusted mortality rates cannot be explained by viral transmission. The synchronized nature of mortality peaks across different regions without expected time delays, and the fact that many countries showed no excess mortality during 2020, provides strong evidence against the viral spread hypothesis. This data pattern suggests other causative factors related to human interventions rather than pathogen transmission.
2. How does aspiration pneumonia differ from transmitted respiratory infections, and why is this distinction significant?
Aspiration pneumonia develops through the inhalation of oropharyngeal or gastric contents into the respiratory tract, representing a self-generated condition that occurs spontaneously within an individual. Unlike transmitted infections, it does not require external pathogen exposure and is particularly common in elderly or vulnerable populations. The condition is influenced by factors such as stress, medical interventions, and environmental conditions that affect the individual's respiratory tract microbiome.
This distinction fundamentally challenges traditional pandemic theories by demonstrating that widespread respiratory disease can occur without person-to-person transmission. The mechanism helps explain how synchronized mortality peaks can occur across different regions without requiring viral spread, and why certain populations, particularly the elderly and those in care facilities, are more vulnerable to severe respiratory conditions during periods of stress or medical intervention.
3. What role does biological stress play in respiratory disease according to Rancourt's analysis?
Biological stress, including psychological stress, functions as a primary driver of disease vulnerability by suppressing immune function and disrupting the body's natural defenses. According to Hans Selye's research, chronic stress can lead to exhaustion-phase collapse of bodily resistance, particularly affecting the respiratory tract microbiome. This stress response can trigger rapid changes in bacterial populations within the lungs, potentially leading to severe infections without external transmission.
The impact becomes especially significant in elderly populations and those with comorbidities, where stress can accelerate existing vulnerabilities. Environmental changes, social isolation, medical interventions, and psychological pressure can create a cascade of biological stress effects that simultaneously impact large populations, explaining synchronized mortality patterns across different regions. This mechanism provides a coherent explanation for how societal disruptions can lead to widespread health impacts without requiring pathogen transmission.
4. How do the spatiotemporal patterns of mortality during 2020-2023 inform our understanding of disease spread?
The spatiotemporal mortality patterns reveal crucial inconsistencies with traditional viral transmission theories. Mortality peaks occurred simultaneously across different regions without showing expected time delays or geographic progression patterns. These peaks did not cross national borders or show typical spread patterns that would be expected with viral transmission, suggesting other causative factors.
The data shows strong temporal associations between mortality peaks and human interventions, such as medical protocols and vaccine rollouts, rather than patterns consistent with pathogen spread. This evidence suggests that institutional responses and medical interventions played a more significant role in mortality patterns than viral transmission, challenging fundamental assumptions about pandemic spread mechanisms.
5. What is the significance of distinguishing between primary and proximal causes of death?
Primary causes represent the hierarchical top-level circumstances or stressors that initiate the chain of events leading to death, while proximal causes are the final medical conditions observed at death. This distinction helps separate underlying causative factors from their ultimate medical manifestations, allowing for a more accurate understanding of what truly drives mortality patterns. Primary causes often relate to environmental, social, or medical interventions that trigger the cascade of events leading to death.
Understanding this difference is crucial for proper analysis of mortality data and development of effective interventions. While death certificates typically focus on proximal causes (like respiratory failure), identifying primary causes (such as stress-induced immunosuppression or medical interventions) provides deeper insight into preventable factors. This framework helps explain how seemingly different medical conditions can share common primary causes, particularly during periods of widespread societal stress or medical intervention.
6. How does Hans Selye's stress research relate to pandemic mortality patterns?
Selye's research established the fundamental role of biological stress in disease development, showing how various stressors can trigger similar physiological responses leading to illness and death. His work demonstrated that chronic stress can cause exhaustion-phase collapse of the body's resistance mechanisms, making individuals more susceptible to various ailments, particularly respiratory conditions. This framework helps explain how societal disruptions and medical interventions can trigger widespread health impacts.
The application of Selye's research to pandemic patterns reveals how synchronized stressors (such as lockdowns, isolation, and medical interventions) can create simultaneous health impacts across populations without requiring pathogen transmission. His work provides a scientific foundation for understanding how psychological and biological stress can function as primary causes of death, particularly when amplified by institutional responses and societal disruptions.
7. What evidence suggests medical interventions may have contributed to excess mortality?
Medical interventions during the pandemic period included widespread use of mechanical ventilation, experimental drug protocols, and denial of standard treatments like antibiotics for pneumonia. Documentation shows that aggressive hospital treatments, particularly during March-May 2020, coincided with mortality peaks. The synchronous timing of these interventions with mortality spikes, and their consistent application across different regions, provides strong evidence of their impact.
The denial of routine medical care, combined with new treatment protocols and experimental interventions, created conditions that could exacerbate existing health vulnerabilities. This included the widespread use of sedatives, changes in standard care protocols, and implementation of isolation measures that could increase stress and vulnerability to conditions like aspiration pneumonia. The temporal alignment between these interventions and mortality peaks, particularly in elderly populations, suggests a causal relationship.
8. How do seasonal mortality patterns relate to the broader theory of transmissionless disease?
Seasonal mortality patterns, particularly winter peaks in respiratory deaths, can be explained through environmental factors rather than viral transmission. These factors include lower temperatures, atmospheric pressure changes, reduced humidity, and altered daylight patterns, all of which can affect respiratory tract health and immune function. The synchronous nature of these seasonal patterns across similar latitude regions supports the theory that environmental conditions, rather than pathogen spread, drive mortality patterns.
The consistency of seasonal mortality patterns across decades, their predictable timing, and their simultaneous occurrence across regions suggest underlying environmental and physiological mechanisms rather than infectious spread. This understanding helps explain how regular seasonal mortality peaks can occur without requiring person-to-person transmission, supporting the broader theory of transmissionless disease development.
9. What role does the respiratory tract microbiome play in disease development?
The respiratory tract microbiome maintains a complex ecosystem of bacteria that can either protect or harm the host depending on environmental conditions and stressors. Research shows that stress, medical interventions, and environmental changes can rapidly alter this microbiome, potentially leading to bacterial overgrowth and pneumonia without requiring external pathogens. This understanding challenges traditional views of respiratory infections as primarily transmitted diseases.
The microbiome's response to stress and environmental changes helps explain how synchronized mortality peaks can occur across populations exposed to similar stressors. When the delicate balance of the respiratory microbiome is disrupted by factors such as isolation, medical interventions, or environmental changes, it can lead to spontaneous bacterial pneumonia, particularly in vulnerable populations. This mechanism provides a scientific basis for understanding how respiratory diseases can develop without transmission.
10. How do social and economic factors influence disease vulnerability?
Social and economic conditions fundamentally shape health outcomes through multiple mechanisms, including access to resources, exposure to stressors, and quality of living conditions. Research shows that populations with lower socioeconomic status experience higher mortality rates during health crises, particularly in urban areas with high population density. These factors create underlying vulnerabilities that can be exacerbated by institutional responses and medical interventions.
The impact of social hierarchy and economic status on health outcomes operates through both direct and indirect pathways, including psychological stress, nutrition, environmental exposure, and access to care. This relationship helps explain why certain populations consistently show higher mortality rates during health crises, independent of pathogen exposure. The strong correlation between socioeconomic factors and mortality patterns supports the understanding of health crises as primarily social and environmental phenomena rather than purely infectious events.
11. What patterns emerged in global mortality data during vaccine rollouts?
Global data analysis revealed consistent temporal associations between COVID-19 vaccine rollouts and increases in excess mortality across different countries. In 100% of countries with sufficient data, significant mortality peaks occurred following vaccine campaigns. Particularly striking was that 97% of countries showed a specific mortality peak in late 2021/early 2022 coinciding with booster rollouts, and 64% showed another peak in late 2022/early 2023 associated with subsequent boosters.
Notably, 30% of countries that had no excess mortality during 2020 only began showing mortality peaks after vaccination programs started. The patterns were particularly pronounced in certain regions, with Australia, Austria, Hong Kong, and several other countries showing especially clear temporal associations between vaccine rollouts and mortality increases. These patterns remained consistent across multiple rounds of vaccination campaigns.
12. How does Rancourt explain the synchronous nature of mortality peaks across different regions?
The synchronous nature of mortality peaks is explained through coordinated institutional responses and widespread environmental stressors rather than pathogen spread. When similar interventions, such as lockdowns, medical protocols, or vaccination campaigns, are implemented across different regions simultaneously, they can trigger similar biological stress responses in vulnerable populations, leading to synchronized health impacts.
This synchronicity is further explained by the concept of transmissionless self-infection, where similar stressors acting on different populations can trigger similar responses in individual respiratory tract microbiomes. The timing of these peaks aligns more closely with human interventions and environmental changes than with patterns expected from pathogen transmission, suggesting that institutional responses and environmental factors drive mortality patterns.
13. What historical evidence supports the theory of transmissionless pandemics?
Historical analysis points to strong associations between major disease outbreaks and societal disruptions, particularly during periods of environmental or economic stress. For example, the great plagues of the Middle Ages coincided with significant economic disruptions and societal collapse, following patterns of class exploitation, money shortages, and widespread poverty. The study of skeletal remains from Black Death victims shows they were developmentally malnourished and in poor health before the outbreak.
Additional historical evidence comes from the correlation between major volcanic eruptions and disease outbreaks over the past 21 centuries. Research indicates that the seven largest dry-fog-producing volcanic explosions coincided with both climatic changes and epidemiological consequences, suggesting environmental factors rather than pathogen spread as primary drivers of historical pandemics.
14. How do care home conditions influence respiratory disease development?
Care home environments create specific vulnerabilities through multiple mechanisms, including the prevalence of dysphagia (swallowing difficulties), malnutrition, and dehydration among residents. These baseline conditions make residents particularly susceptible to aspiration pneumonia and other respiratory complications, especially when routine care patterns are disrupted or modified by new protocols or staffing changes.
The impact of care home conditions becomes especially significant during periods of institutional stress, when changes in staffing, isolation protocols, or medical interventions can disrupt established care routines. Factors such as reduced mobility, increased isolation, and changes in medication protocols can trigger cascading health impacts, particularly through mechanisms like aspiration pneumonia, without requiring pathogen transmission between residents.
15. What is the relationship between psychological stress and immune response?
Psychological stress directly impacts immune function through multiple pathways, including immunosuppression and altered inflammatory responses. Research demonstrates that chronic psychological stress can significantly increase susceptibility to respiratory infections, with social isolation and fear being particularly potent stressors. The relationship operates through known psychoneuroimmunological mechanisms that connect mental states to physical health outcomes.
The impact becomes especially significant when psychological stress is amplified by social conditions and institutional responses. Mass communication of fear and uncertainty, combined with isolation measures and disruption of normal social patterns, can create widespread stress responses that synchronously affect population health. This mechanism helps explain how coordinated institutional responses can trigger simultaneous health impacts across different populations.
16. How does age factor into stress-related disease vulnerability?
Age significantly amplifies the impact of biological stress through multiple mechanisms, including reduced physiological resilience and increased immunosuppressive activity. Elderly individuals show greater vulnerability to stress-induced health impacts, particularly in their respiratory systems. This vulnerability increases exponentially with age, explaining why mortality patterns during health crises show strong age-dependent effects.
The age factor becomes particularly significant in institutional settings, where elderly individuals face multiple compounding stressors. Research shows that aging populations have reduced capacity to maintain homeostasis under stress, making them especially vulnerable to disruptions in care routines, environmental changes, and medical interventions. This explains why elderly populations consistently show the highest mortality rates during health crises, independent of pathogen exposure.
17. What role do environmental factors play in disease development?
Environmental factors directly influence disease development through multiple mechanisms, including effects on respiratory tract microbiome, immune function, and physiological stress responses. Winter conditions, in particular, create specific vulnerabilities through reduced temperatures, altered atmospheric pressure, lower humidity, and changed oxygen partial pressures, all of which can affect respiratory health independently of pathogen transmission.
The impact of environmental factors explains regular seasonal mortality patterns and helps account for synchronized health impacts across similar geographic regions. These factors can trigger simultaneous biological responses across populations exposed to similar conditions, helping to explain how respiratory diseases can develop and spread without requiring person-to-person transmission of pathogens.
18. How does Rancourt explain the relationship between tuberculosis and socioeconomic conditions?
Tuberculosis serves as a model for understanding how socioeconomic conditions shape disease patterns through mechanisms independent of simple transmission. While traditionally viewed as a transmissible disease, tuberculosis shows strong associations with living conditions, population density, and economic status, suggesting that social and environmental factors play crucial roles in disease development and progression.
Research indicates that about one-third of the world's population carries the TB pathogen, yet active disease development correlates strongly with social and environmental stressors rather than just exposure. This relationship helps explain mortality patterns during the COVID period, where similar socioeconomic factors influenced disease outcomes, suggesting that social conditions rather than pathogen transmission may be the primary driver of disease development.
19. What evidence supports the connection between medical interventions and mortality rates?
Data shows strong temporal correlations between specific medical interventions and mortality peaks, particularly during the early pandemic period. The widespread use of mechanical ventilation, experimental drug protocols, and changes in standard care practices coincided with significant increases in mortality. Documentation of these interventions, combined with their timing and geographic distribution, provides strong evidence for their role in excess deaths.
The impact of medical interventions is further supported by data showing how changes in treatment protocols, including the denial of standard treatments like antibiotics for pneumonia, coincided with mortality increases. The synchronous implementation of these interventions across different regions, combined with their temporal association with mortality peaks, suggests a causal relationship between medical protocols and excess deaths.
20. How does social dominance hierarchy affect health outcomes?
Social dominance hierarchy influences health through multiple mechanisms, including stress responses, access to resources, and vulnerability to institutional impacts. Research shows that position within social hierarchies significantly affects individual health outcomes, with those in subordinate positions experiencing greater biological stress and reduced capacity to cope with environmental changes or medical interventions.
This hierarchical effect becomes particularly significant during health crises, when institutional responses often disproportionately impact those in lower social positions. The relationship helps explain why mortality patterns during the COVID period showed strong correlations with social and economic status, suggesting that health outcomes are primarily determined by social position rather than pathogen exposure.
What is the significance of medieval plague economic patterns in understanding modern pandemics?
Medieval plague patterns followed specific economic sequences: growing class exploitation led to money shortages, which triggered rising living costs, resulting in widespread poverty and subsequent health consequences. This historical pattern reveals how economic cycles and social collapse preceded and potentially caused disease outbreaks, rather than the reverse. Forensic analysis of Black Death victims' skeletons confirms they were developmentally malnourished before the outbreak.
These historical patterns mirror modern pandemic dynamics, where economic disruptions and social stressors precede health crises. The medieval evidence suggests that pandemics may be consequences of societal collapse rather than their cause, providing insight into how modern economic disruptions and social stress might trigger similar health outcomes through biological stress mechanisms.
22. How do volcanic eruptions relate to historical pandemic patterns?
Research examining the seven largest dry-fog-producing volcanic explosions over 21 centuries found strong temporal associations between these events and subsequent epidemics. This correlation was deemed "very unlikely coincidence" by researchers, suggesting environmental factors play a crucial role in triggering widespread health impacts. The volcanic events created specific atmospheric conditions affecting temperature, humidity, and potentially toxic emissions.
These historical observations support the broader theory that environmental changes can trigger synchronized health impacts across populations without requiring pathogen transmission. The volcanic evidence demonstrates how large-scale environmental disruptions can create conditions leading to widespread disease, supporting modern theories about environmental triggers for health crises.
23. What role does the gut and respiratory microbiome play in disease development?
The respiratory tract maintains a complex microbiome that can shift from protective to harmful depending on environmental conditions and stressors. Current research shows that rather than being sterile, lungs contain diverse bacterial communities that respond dynamically to environmental changes. Stress, medical interventions, or environmental factors can trigger rapid shifts in these microbial populations, potentially leading to severe respiratory conditions without external pathogens.
This understanding challenges traditional assumptions about lung sterility and disease development. The microbiome can undergo rapid changes through positive feedback loops, where stress or environmental factors trigger shifts from diverse bacterial communities to dominance by single species. This mechanism explains how respiratory diseases can develop spontaneously within individuals when their microbiome balance is disrupted.
24. How do institutional messaging and fear affect population health outcomes?
Institutional messaging during health crises can create widespread psychological stress through fear amplification and social disruption. This messaging, when coordinated across different regions, can trigger simultaneous stress responses in populations, leading to synchronized biological impacts. The effect becomes self-reinforcing through social transmission and positive feedback mechanisms.
The impact of fear-based messaging is particularly significant when combined with isolation measures and social disruption. This combination creates conditions for collective stress amplification, where individual biological responses are magnified by social factors. The synchronized nature of these effects helps explain how institutional responses can trigger simultaneous health impacts across different populations.
25. What evidence exists regarding the impact of lockdowns on mortality?
Lockdown measures created multiple pathways for health impacts, including increased isolation, reduced mobility, and disrupted access to routine care. The timing of lockdown implementations shows strong correlations with mortality increases, particularly in vulnerable populations. The effects were most pronounced in settings where isolation measures were strictly enforced, such as care homes and medical facilities.
The impact of lockdowns varied significantly based on socioeconomic status, with more severe effects in populations lacking resources to mitigate isolation impacts. This variation helps explain mortality patterns that showed strong correlations with social and economic factors rather than viral exposure. The evidence suggests lockdowns functioned as primary stressors triggering biological stress responses in vulnerable populations.
26. How do winter conditions influence respiratory disease development?
Winter conditions create specific physiological challenges through multiple mechanisms, including lower temperatures, reduced atmospheric humidity, larger atmospheric pressure variations, and changed oxygen partial pressures. These environmental factors directly affect respiratory tract health and immune function, creating conditions favorable for respiratory disease development without requiring pathogen transmission.
The seasonal pattern of winter mortality peaks can be explained through these environmental mechanisms rather than infectious spread. The synchronous nature of these effects across similar latitude regions supports environmental rather than transmission-based explanations for seasonal mortality patterns. This understanding helps explain regular winter mortality peaks without requiring person-to-person transmission theories.
27. What patterns emerged in care home mortality during the pandemic period?
Care home mortality showed distinct patterns related to institutional interventions and changes in care protocols. Pre-existing conditions in care homes, including widespread malnutrition and dehydration, created baseline vulnerabilities that were exacerbated by pandemic responses. The implementation of new protocols, staffing changes, and isolation measures coincided with significant mortality increases.
These patterns were particularly pronounced when care homes experienced disruptions to routine care, increased isolation measures, or changes in medical protocols. The timing and nature of these mortality increases suggest they were primarily driven by institutional responses rather than pathogen spread, as evidenced by the synchronous nature of mortality peaks across different facilities implementing similar measures.
28. How does Rancourt explain the relationship between vaccination campaigns and mortality trends?
Analysis of mortality data from multiple countries shows consistent temporal associations between vaccine rollout periods and increases in excess mortality. These associations were particularly strong during rapid rollout periods and booster campaigns, with 97% of countries showing specific mortality peaks coinciding with late-2021 booster programs. The patterns were especially clear in countries that had no excess mortality before vaccination campaigns began.
The relationship between vaccination campaigns and mortality trends showed specific characteristics, including age-stratified effects and dose-dependent patterns. The timing and nature of these associations remained consistent across different countries and regions, suggesting systematic rather than coincidental relationships. The patterns were particularly pronounced in certain regions where rapid rollout programs were implemented.
29. What role do diagnostic practices play in mortality statistics?
Diagnostic practices during the pandemic period showed systematic biases that influenced mortality statistics. The widespread implementation of new testing protocols and diagnostic criteria created patterns that aligned more closely with institutional responses than with disease spread. These practices influenced both treatment decisions and mortality classifications, creating feedback loops between diagnosis and outcomes.
The impact of diagnostic practices becomes particularly significant when considering the denial of standard treatments based on test results. The relationship between diagnostic protocols and mortality statistics suggests that testing and classification systems played an active role in shaping health outcomes rather than merely recording them. This understanding helps explain how institutional practices contributed to mortality patterns.
30. How does Rancourt explain mortality variations between Eastern and Western European countries?
Mortality variations between Eastern and Western Europe showed distinct patterns related to pre-existing health system differences and socioeconomic factors. These variations correlated strongly with historical tuberculosis prevalence, suggesting underlying social and economic factors played crucial roles in determining health outcomes. The differences remained consistent throughout the pandemic period, indicating structural rather than pathogen-related causes.
These regional variations provide important evidence for understanding how social and economic factors influence health outcomes during crises. The persistent nature of these differences, despite similar viral exposure opportunities, supports theories emphasizing social and environmental factors over transmission-based explanations for mortality patterns.
31. What evidence supports the stress-induced immunosuppression hypothesis?
Recent animal studies demonstrate that even single episodes of restraint and immobilization stress can cause severe immunosuppression, more significantly than other stressors. Research shows stressed animals experience significant spleen macrophage cell death and reduced ability to defend against bacterial challenges. These findings directly parallel observations of human responses to confinement and isolation measures during the pandemic period.
Psychological stress demonstrates measurable impacts on immune function through established psychoneuroimmunological pathways. Studies dating back to Selye's original work show how chronic stress leads to exhaustion-phase collapse of bodily resistance, making individuals more susceptible to infections from their own microbiome. This mechanism explains how synchronized stressors can trigger simultaneous health impacts across populations.
32. How do socioeconomic factors influence pandemic vulnerability?
Socioeconomic conditions create fundamental differences in ability to cope with pandemic measures and health stressors. Those with higher socioeconomic status maintained access to resources like comfortable housing, remote work options, private exercise facilities, and continued healthcare access. In contrast, lower socioeconomic groups faced compounded stressors from job loss, crowded living conditions, and disrupted access to basic services.
The impact of these differences became particularly evident in urban regions with high poverty and population density, where mortality rates showed strong correlations with economic status. These patterns remained consistent across different countries and regions, suggesting that social and economic factors, rather than viral exposure, primarily determined health outcomes during the pandemic period.
33. What role do antibiotics and treatment protocols play in mortality outcomes?
The systematic denial of antibiotic treatments for bacterial pneumonia during the pandemic period represents a significant shift in medical practice that coincided with increased mortality. This change in protocol occurred despite evidence that more than half of severe respiratory cases involved bacterial co-infections. The withholding of standard treatments, particularly antibiotics, potentially allowed treatable conditions to become fatal.
Treatment protocols focused on viral interventions while overlooking bacterial pneumonia, especially aspiration pneumonia, which is a leading cause of death in elderly populations. This shift in focus led to the undertreatment of bacterial infections, creating conditions where normally manageable respiratory conditions became life-threatening, particularly in care home settings and among vulnerable populations.
34. How does Rancourt explain the relationship between hospital protocols and mortality rates?
Hospital protocols during the pandemic period included widespread use of mechanical ventilation, experimental drug treatments, and new sedation protocols that coincided with mortality increases. These interventions, particularly early aggressive ventilation and strong sedation, created conditions that could increase the risk of complications like ventilator-associated pneumonia and aspiration pneumonia.
The implementation of these protocols showed strong temporal associations with mortality peaks, especially during the March-May 2020 period. The aggressive nature of these interventions, combined with the denial of standard treatments, created a medical environment where institutional responses potentially contributed to, rather than mitigated, patient mortality.
35. What evidence supports the transmissionless bacterial pneumonia hypothesis?
Current scientific understanding of the lung microbiome shows that it contains diverse bacterial communities capable of rapid shifts into pathogenic states without external transmission. Research demonstrates that stress, medical interventions, and environmental changes can trigger these shifts, leading to severe respiratory infections developing spontaneously within individuals.
This mechanism is particularly evident in cases of aspiration pneumonia, where bacterial infections develop without person-to-person transmission. The widespread prevalence of these conditions, especially in elderly and vulnerable populations, provides a plausible mechanism for synchronized respiratory disease outbreaks without requiring viral spread.
36. How do geographic and demographic factors influence mortality patterns?
Geographic factors, including latitude and environmental conditions, show strong correlations with mortality patterns, particularly in seasonal variations. These patterns demonstrate synchronicity across similar latitudes without evidence of spread between regions, suggesting environmental rather than transmission-based mechanisms.
Demographic factors, especially age and socioeconomic status, show consistent relationships with mortality rates across different regions. The exponential increase in mortality risk with age, combined with social and economic vulnerabilities, creates distinct patterns that align more closely with environmental and institutional factors than with pathogen exposure.
37. What role does population density play in mortality outcomes?
Population density correlates strongly with mortality rates, particularly in urban areas with high poverty levels. However, this relationship appears mediated through social and economic factors rather than increased transmission opportunities. The most intense mortality peaks occurred in urban regions with high poverty and population density, yet similar density areas with better socioeconomic conditions often showed lower impact.
The relationship between population density and mortality becomes particularly significant when combined with other social stressors and institutional responses. This suggests that density effects operate primarily through social and environmental mechanisms rather than through increased pathogen transmission opportunities.
38. How does Rancourt explain the relationship between medical testing and mortality?
Medical testing protocols during the pandemic period created feedback loops between diagnosis and treatment decisions, potentially leading to inappropriate interventions. The widespread use of PCR testing, despite questions about its reliability, influenced treatment decisions and contributed to the denial of standard treatments for bacterial infections.
The implementation of aggressive testing programs coincided with changes in treatment protocols and mortality increases. This relationship suggests that testing practices played an active role in shaping health outcomes by influencing treatment decisions and institutional responses, rather than simply detecting disease presence.
39. What evidence supports the connection between institutional responses and mortality rates?
Strong temporal correlations exist between coordinated institutional responses and mortality peaks across different regions. The synchronized nature of these responses, including lockdowns, treatment protocols, and vaccination campaigns, aligns closely with mortality patterns in ways that cannot be explained by viral transmission.
The impact of institutional responses becomes particularly evident in cases where similar interventions produced similar mortality patterns across different regions simultaneously. This synchronicity, combined with the lack of evidence for viral spread patterns, suggests that institutional responses themselves functioned as primary drivers of mortality outcomes.
40. How does Rancourt explain the role of environmental factors in seasonal mortality patterns?
Environmental factors create specific physiological challenges through multiple mechanisms, including temperature variations, atmospheric pressure changes, and humidity levels. These factors directly affect respiratory tract health and immune function in ways that can trigger synchronized health impacts across populations exposed to similar conditions.
The predictable nature of seasonal mortality patterns, particularly winter peaks in respiratory deaths, can be explained through these environmental mechanisms rather than requiring transmission-based explanations. This understanding helps account for the synchronized nature of seasonal mortality patterns across similar latitude regions without requiring person-to-person transmission theories.
I appreciate you being here.
If you've found the content interesting, useful and maybe even helpful, please consider supporting it through a small paid subscription. While everything here is free, your paid subscription is important as it helps in covering some of the operational costs and supports the continuation of this independent research and journalism work. It also helps keep it free for those that cannot afford to pay.
Please make full use of the Free Libraries.
Unbekoming Interview Library: Great interviews across a spectrum of important topics.
Unbekoming Book Summary Library: Concise summaries of important books.
Stories
I'm always in search of good stories, people with valuable expertise and helpful books. Please don't hesitate to get in touch at unbekoming@outlook.com
For COVID vaccine injury
Consider the FLCCC Post-Vaccine Treatment as a resource.
Baseline Human Health
Watch and share this profound 21-minute video to understand and appreciate what health looks like without vaccination.




There is no proof that pandemics are real and therefore you need not stress over their non-existence. Contagion is a crock of fear with the express purpose of promoting Pig Pharma drugs and vaccines which will give you no solace.
Wow wow wow. I love this exploration and explanation of the ideas in my recent medical hypothesis paper. Well done. Thanks for proving that that my paper is understood! Cheers, DR